Are Endometriosis, Adenomyosis, and PCOS Autoimmune Conditions?
By Our Daughters Foundation
More and more women are asking an important question: Could my hormone-related illness also be connected to my immune system?
Conditions like endometriosis, adenomyosis, and polycystic ovary syndrome (PCOS) are often discussed in the context of reproductive health or hormonal imbalance. But researchers are beginning to explore deeper connections—specifically, whether autoimmunity plays a role in these diseases.
Let’s break down what the science says—and what questions remain unanswered.
Are Endometriosis, Adenomyosis, and PCOS Autoimmune Conditions?
By Our Daughters Foundation
More and more women are asking an important question: Could my hormone-related illness also be connected to my immune system?
Conditions like endometriosis, adenomyosis, and polycystic ovary syndrome (PCOS) are often discussed in the context of reproductive health or hormonal imbalance. But researchers are beginning to explore deeper connections—specifically, whether autoimmunity plays a role in these diseases.
Let’s break down what the science says—and what questions remain unanswered.
What Is Autoimmunity?
The immune system is designed to protect the body from threats like viruses and bacteria. But in autoimmune diseases, the immune system becomes misguided and starts attacking the body’s own cells and tissues.
Common autoimmune conditions include:
• Lupus
• Rheumatoid arthritis
• Hashimoto’s thyroiditis
• Multiple sclerosis
Symptoms vary widely, but many autoimmune conditions involve chronic inflammation, pain, fatigue, and a pattern of flare-ups.

The Immune System and Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus—causing pain, inflammation, and sometimes infertility. While its exact cause is still debated, many researchers believe that the immune system fails to clear out these rogue cells effectively.
Several studies have found:
• Women with endometriosis often have higher levels of inflammatory markers, like cytokines and prostaglandins.
• Natural killer (NK) cell activity is lower in women with endometriosis, impairing the immune system’s ability to destroy misplaced cells.
• There are elevated autoantibodies in some patients, suggesting an autoimmune component.
Some scientists now consider endometriosis to be a non-classical autoimmune disease—showing many features of one without meeting all diagnostic criteria.
Further reading:
• NIH - Immune dysfunction in endometriosis: https://pubmed.ncbi.nlm.nih.gov/30664929/
• Cleveland Clinic - Endometriosis and the Immune System: https://health.clevelandclinic.org/endometriosis-and-the-immune-system/
What About Adenomyosis?
Adenomyosis is sometimes called the "sister disease" of endometriosis. It occurs when endometrial tissue grows into the muscular wall of the uterus. It's less studied, but immune abnormalities have also been observed.
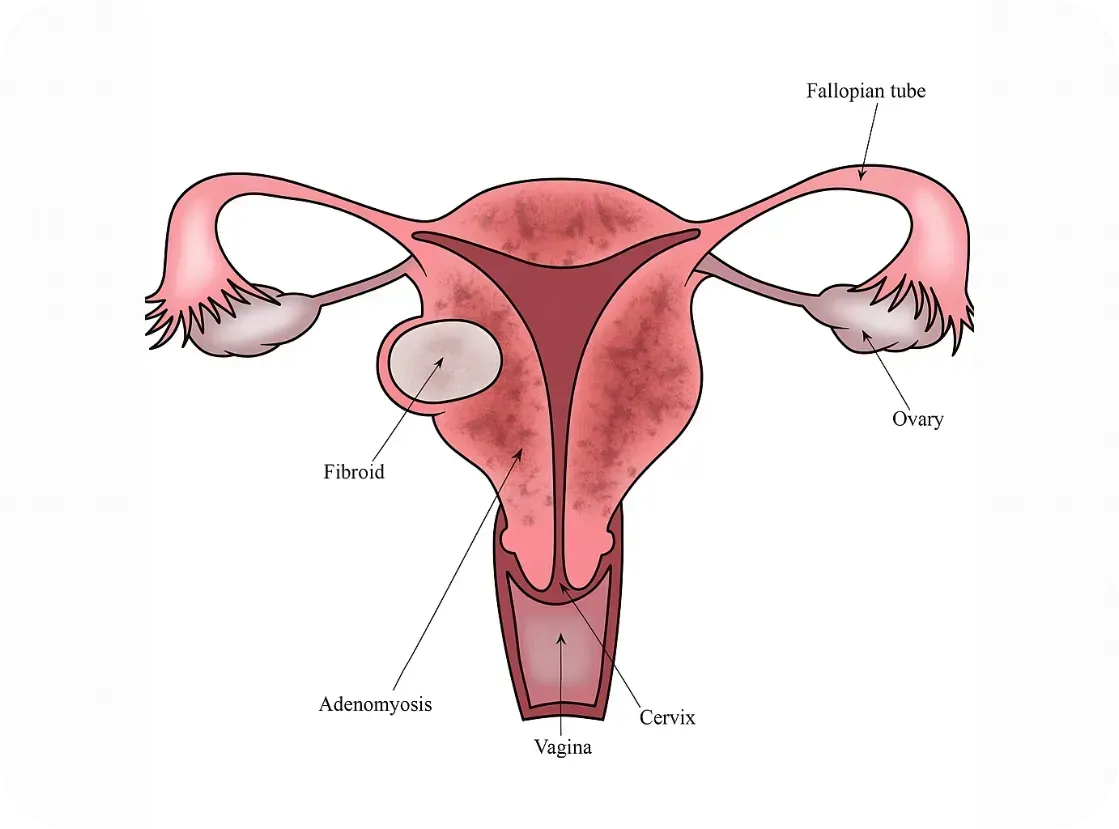
Research is still emerging, but here’s what we know:
• Women with adenomyosis show immune cell changes and chronic inflammation within the uterus.
• Some studies report increased macrophage and mast cell activity—cells involved in both immune defense and inflammation
• The condition often coexists with endometriosis, raising questions about shared immune pathways.
While it’s too early to label adenomyosis an autoimmune disorder, it may involve an immune imbalance that contributes to symptoms.
Further reading:
• Frontiers in Immunology - Immunopathogenesis of Adenomyosis: https://www.frontiersin.org/articles/10.3389/fimmu.2021.796273/full
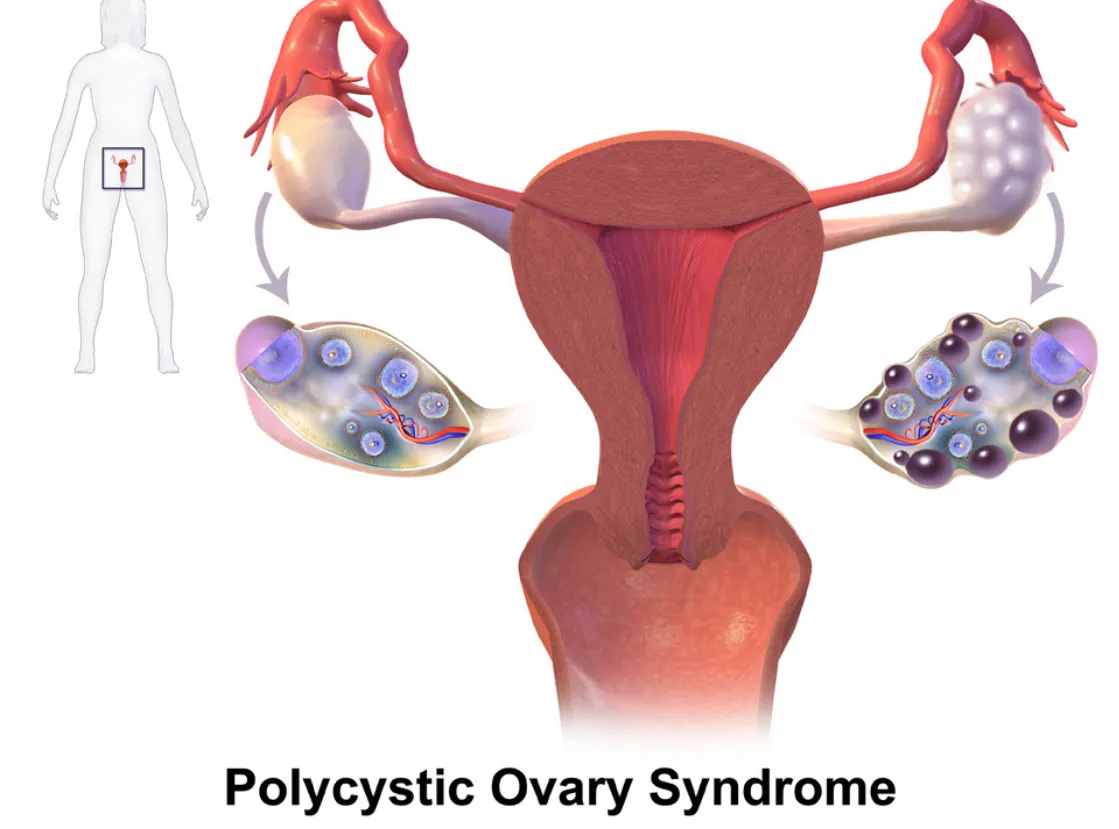
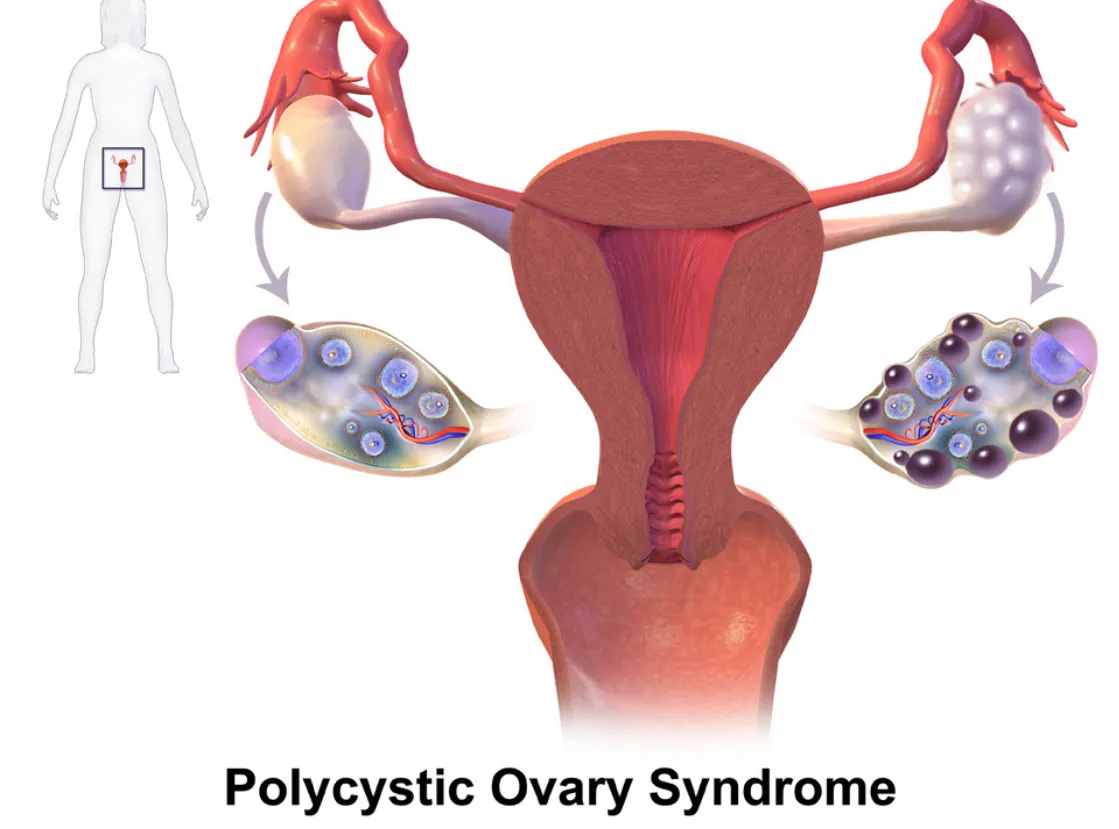
PCOS and Autoimmune Overlap
Polycystic ovary syndrome (PCOS) is primarily known as a hormonal disorder involving androgen excess and insulin resistance. However, there’s growing interest in its immune connections, especially in women with chronic inflammation or thyroid issues.
Emerging links include:
• Hashimoto’s thyroiditis (an autoimmune thyroid disorder) is more common in women with PCOS.
• Inflammatory markers like C-reactive protein (CRP) are often elevated in PCOS patients.
• Some PCOS patients have anti-ovarian antibodies, suggesting potential autoimmunity.
Still, the autoimmune theory is more speculative in PCOS than in endometriosis.
Further reading:
Further reading:
• Journal of Clinical Endocrinology & Metabolism - PCOS and Autoimmune Disease: https://academic.oup.com/jcem/article/106/9/e3536/6280755
Why Does This Matter?
If immune dysfunction is part of the puzzle, treatment strategies may need to shift. Many women with endometriosis, adenomyosis, or PCOS are treated solely with hormone suppression—but if autoimmunity is involved, we may also need to address inflammation, gut health, and immune regulation.
There’s also hope that newer treatments—like immunomodulatory therapies or even personalized nutrition and lifestyle interventions—could improve outcomes when tailored to the immune system’s role.
Bottom Line
We don’t yet have all the answers, but the research is evolving. Endometriosis, adenomyosis, and PCOS may not be traditional autoimmune diseases—but they often coexist with immune dysfunction, and the overlap deserves attention. At Our Daughters Foundation, we believe in honoring women’s voices, advocating for deeper research, and pursuing whole-body solutions.
If you’ve experienced overlapping conditions like endo, thyroid disease, or unexplained inflammation—you’re not alone.
What Is Autoimmunity?
The immune system is designed to protect the body from threats like viruses and bacteria. But in autoimmune diseases, the immune system becomes misguided and starts attacking the body’s own cells and tissues.
Common autoimmune conditions include:
• Lupus
• Rheumatoid arthritis
• Hashimoto’s thyroiditis
• Multiple sclerosis
Symptoms vary widely, but many autoimmune conditions involve chronic inflammation, pain, fatigue, and a pattern of flare-ups.

The Immune System and Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus—causing pain, inflammation, and sometimes infertility. While its exact cause is still debated, many researchers believe that the immune system fails to clear out these rogue cells effectively.
Several studies have found:
• Women with endometriosis often have higher levels of inflammatory markers, like cytokines and prostaglandins.
• Natural killer (NK) cell activity is lower in women with endometriosis, impairing the immune system’s ability to destroy misplaced cells.
• There are elevated autoantibodies in some patients, suggesting an autoimmune component.
Some scientists now consider endometriosis to be a non-classical autoimmune disease—showing many features of one without meeting all diagnostic criteria.
Further reading:
• NIH - Immune dysfunction in endometriosis: https://pubmed.ncbi.nlm.nih.gov/30664929/
• Cleveland Clinic - Endometriosis and the Immune System: https://health.clevelandclinic.org/endometriosis-and-the-immune-system/
What About Adenomyosis?
Adenomyosis is sometimes called the "sister disease" of endometriosis. It occurs when endometrial tissue grows into the muscular wall of the uterus. It's less studied, but immune abnormalities have also been observed.
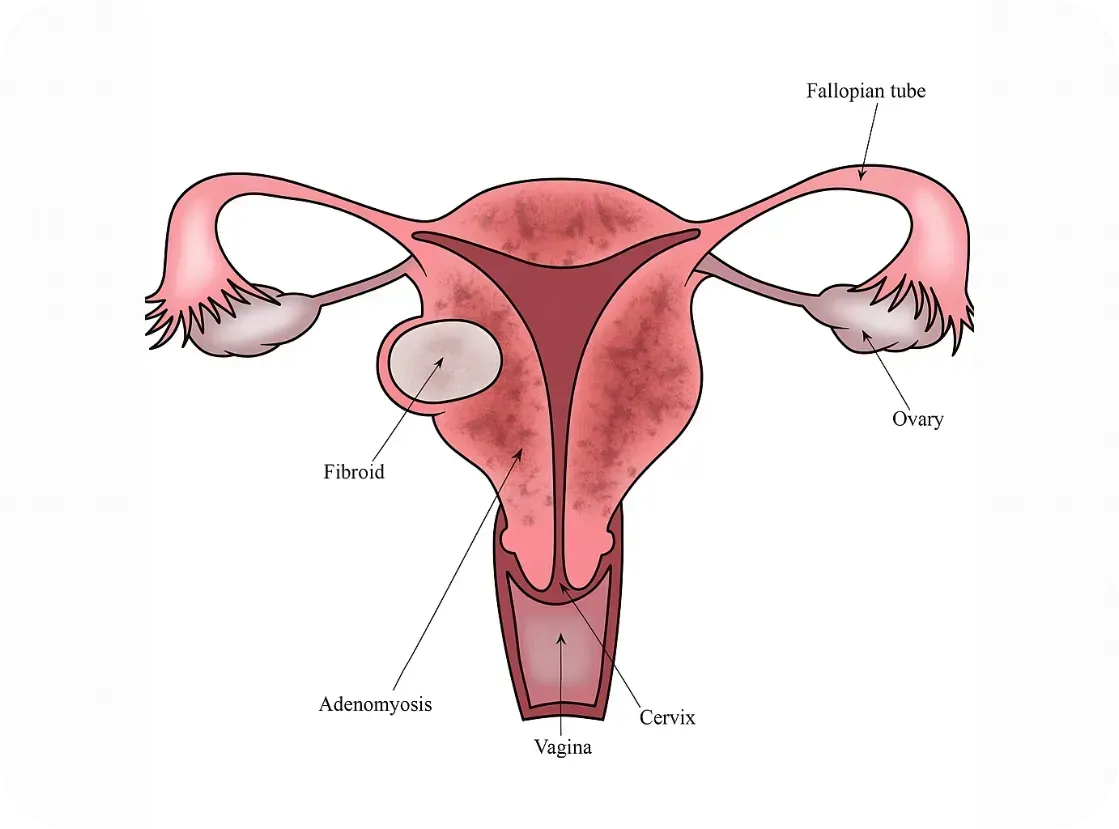
Research is still emerging, but here’s what we know:
• Women with adenomyosis show immune cell changes and chronic inflammation within the uterus.
• Some studies report increased macrophage and mast cell activity—cells involved in both immune defense and inflammation
• The condition often coexists with endometriosis, raising questions about shared immune pathways.
While it’s too early to label adenomyosis an autoimmune disorder, it may involve an immune imbalance that contributes to symptoms.
Further reading:
• Frontiers in Immunology - Immunopathogenesis of Adenomyosis: https://www.frontiersin.org/articles/10.3389/fimmu.2021.796273/full
PCOS and Autoimmune Overlap
Polycystic ovary syndrome (PCOS) is primarily known as a hormonal disorder involving androgen excess and insulin resistance. However, there’s growing interest in its immune connections, especially in women with chronic inflammation or thyroid issues.
Emerging links include:
• Hashimoto’s thyroiditis (an autoimmune thyroid disorder) is more common in women with PCOS.
• Inflammatory markers like C-reactive protein (CRP) are often elevated in PCOS patients.
• Some PCOS patients have anti-ovarian antibodies, suggesting potential autoimmunity.
Still, the autoimmune theory is more speculative in PCOS than in endometriosis.
Further reading:
Further reading:
• Journal of Clinical Endocrinology & Metabolism - PCOS and Autoimmune Disease: https://academic.oup.com/jcem/article/106/9/e3536/6280755
Why Does This Matter?
If immune dysfunction is part of the puzzle, treatment strategies may need to shift. Many women with endometriosis, adenomyosis, or PCOS are treated solely with hormone suppression—but if autoimmunity is involved, we may also need to address inflammation, gut health, and immune regulation.
There’s also hope that newer treatments—like immunomodulatory therapies or even personalized nutrition and lifestyle interventions—could improve outcomes when tailored to the immune system’s role.
Bottom Line
We don’t yet have all the answers, but the research is evolving. Endometriosis, adenomyosis, and PCOS may not be traditional autoimmune diseases—but they often coexist with immune dysfunction, and the overlap deserves attention. At Our Daughters Foundation, we believe in honoring women’s voices, advocating for deeper research, and pursuing whole-body solutions.
If you’ve experienced overlapping conditions like endo, thyroid disease, or unexplained inflammation—you’re not alone.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.

Follow the Money: We Can Do Better

I want to start by saying: this post is not political. This post is about our shared experiences as women—as a mother of three daughters, a grandmother, and a friend to countless women who have been frustrated and overwhelmed by the current state of our medical system.
We have a common experience—and it needs to be heard and shared.
I was encouraged to write this after reading that the Gates Foundation just pledged $2.5 billion toward women’s health initiatives. But reading the accompanying article published in STAT left me deeply frustrated. The statistics on women’s health haven’t improved enough.
“The Gates Foundation said the goal of the new initiative is to address a long-running deficit in medicine that has disfavored women’s health—to the extent that the ‘typical’ patient described to medical students has traditionally been male.”
— STAT News
In a BMJ article published last week, Ru Cheng, the foundation’s Director of Women’s Health Initiatives, shared that only 1% of global research and development funding is allocated to women’s health issues outside of oncology, and between 2013 and 2023, only 8.8% of NIH-funded research focused exclusively on women.
These are not opinions. These are widely reported, peer-reviewed statistics from respected medical journals. And this is why women with Endometriosis or Adenomyosis are subjected to 8-10 years of medical gaslighting before they are diagnosed. And this is why women with these diseases literally need to be cut open in order to diagnose their disease. It's just not acceptable that laparoscopic surgery is required for diagnosis in 2025. We should be much further along by now. Do you realize that most endometriosis lesions cannot be detected on scans or imaging? I know this can be figured out! Progress is being made, let's push it along.
Men’s and women’s health issues are not treated with the same urgency or investment. That’s not a radical feminist opinion or a political talking point—it’s a follow-the-dollars reality.
The gaslighting women experience around this issue doesn’t just come from doctors. I’ve had people close to me—both men and women—try to argue that women’s health isn’t being overlooked, that maybe we’re exaggerating. But the data is undeniable.
If our mothers, daughters, grandmothers, aunts, and female friends matter—if we believe them and value their lives—then it’s time to stop dismissing their pain. It’s time to pay attention to the statistics, follow the funding, and change our course.
That’s why we launched Our Daughters Foundation:
To fight for awareness, raise money for research, and provide visibility and hope.
When we first started on this path of setting up the foundation, I was shocked to learn that women weren’t even included in NIH-funded medical trials until 1993. That wasn’t so long ago. If you’re close to my age, that year probably feels recent (Jurassic Park was in theaters and Bill Clinton was president). Incredibly, only 1% of non-cancer healthcare R&D currently targets female-specific conditions.
The Gates initiative is a huge step—but it’s not enough.
Women are still underrepresented in studies involving pain management, cardiovascular disease, and autoimmune conditions—fields where female biology plays a huge role in how we experience disease and respond to treatment. Even more disturbing is the lack of research funding for diseases that exclusively affect women, like endometriosis, adenomyosis, PCOS, and uterine fibroids. These are not rare diseases and conditions, and for many women, they’re life-altering.
For Those Suffering Now...and Our Daughters in the Future
I hope you’ll join us in raising awareness about the women’s health conditions that affect the people we love—and the people you love. These women are not statistics. They’re not being “dramatic” or “too emotional.” They are Mom, Nana, Auntie, Daughter, Friend.
As always, I’ve included data and references for everything I’ve shared above. (Again—thank you, ChatGPT, for helping curate these.) Please see the resources and stats below, which paint a clear picture of the disparities we’re up against.
— There is so much more to say, & even more that we can DO! Please help us make some noise!
With gratitude,
Kara
A Quick History Review
Thanks to ChatGPT research, here’s a timeline that puts things in perspective:1977 – The FDA banned women of childbearing age from participating in early drug trials. The reason? Hormonal “complexity” and fear of pregnancy-related liability (like the thalidomide crisis). That meant chemotherapy, heart meds, pain relief—all tested mostly on men.
1986–1987: The NIH began encouraging researchers to include women in funded studies. This was first published in the NIH Guide for Grants and Contracts
1993 – The NIH Revitalization Act required federally funded trials to finally include women and analyze sex-based differences.
The Pain Gap
Women experience chronic pain more frequently than men, but they’re still less likely to be treated seriously. A 2020 study of over 200,000 patients found:
Women consistently face longer delays and lower diagnostic accuracy than men—even for the same symptoms.
Women are:
Less likely to receive pain medication in the ER
Made to wait an average of 16 minutes longer
More likely to be told their symptoms are “psychological”
Despite the fact that 70% of chronic pain patients are women, 80% of pain research is still done on male animals or male subjects.
Let that sink in.

Sources
Reuters – Gates Foundation’s $2.5B women’s health initiative
STAT News: Women’s health funding still ignored
FDA 1977 guidance
NIH Revitalization Act
Medidata: History of women in clinical trials
NIH: Endometriosis Funding Summary
SELF: The PCOS Medical Mystery
New Security Beat: VC funding comparison
Statista: Hair Loss Pharma Market
RAND + WHAM Study on Economic Return
NIH: Gender Bias in ER Pain Treatment
Scientific American: Sex Bias in Pain Research
