GUT FEELINGS: The Hidden Link Between Gut Health and Hormonal Imbalance
By Our Daughters Foundation
GUT FEELINGS: The Hidden Link Between Gut Health and Hormonal Imbalance
By Our Daughters Foundation
1. The Gut Microbiome: Your Internal Ecosystem
Your gut isn’t just a tube for digesting food. It’s home to trillions of bacteria that:
• Help break down food
• Make key nutrients (like B vitamins)
• Train your immune system
• And — importantly — regulate estrogen levels
This bacterial community is called the gut microbiome, and when it’s healthy and diverse, it supports balanced hormones. But when the microbiome is out of balance — a condition called dysbiosis — problems can arise.
2. Estrobolome: The Gut’s Hormone Filte
Inside the gut, a specific group of bacteria known as the estrobolome helps process estrogen. These bacteria produce enzymes (like beta-glucuronidase) that influence how much estrogen is reabsorbed into the bloodstream versus excreted.
When the estrobolome is overactive or underactive, it can lead to:
• Excess circulating estrogen → linked to endometriosis, fibroids, PMS, and breast tendernes
• Too little estrogen → contributing to mood changes, bone loss, and vaginal dryness
So a disrupted gut can directly amplify hormonal imbalances.
3. Inflammation: The Common Denominator
Both gut dysbiosis and endometriosis are associated with chronic inflammation. When the gut barrier is weakened (a condition sometimes called “leaky gut”), it allows inflammatory molecules to pass into the bloodstream. This triggers an immune response — and in people with endometriosis or PCOS, it can worsen pelvic pain, fatigue, and hormonal chaos.

4. What the Research Says
While this field is still developing, early studies have found:
• Women with endometriosis often have altered gut microbiomes compared to those without the condition. [Study: Ata et al., 2019, Scientific Reports]
• A high-fiber, plant-rich diet may help support a more balanced gut flora and improve estrogen metabolism. [Study: Fuhrman et al., 2004, Journal of Nutrition]
• Some researchers are exploring probiotic therapy as a future tool for managing hormone-related conditions.
5. What Can You Do?
You can’t fully control your hormones — but you can support your gut.
Here are some gut-friendly, hormone-supporting habits:
• Eat more fiber: vegetables, fruits, legumes, and seeds
• Avoid excessive sugar and processed foods
• Include fermented foods: yogurt, kefir, sauerkraut, kimchi
• Consider a probiotic — talk to your provider first
• Manage stress — cortisol (the stress hormone) also affects gut balance
• Support liver detoxification (which works with your gut to clear estrogen): eat cruciferous vegetables like broccoli and cauliflower

Final Thoughts
The gut isn’t just about digestion — it’s a key player in how your body handles hormones, pain, and inflammation.
If you’re struggling with endometriosis, PCOS, or unexplained hormone symptoms, supporting your gut might be an empowering place to start.
Want to Learn More?
Here are some helpful articles and research:
• The Gut Microbiome and Estrogen Metabolism – NIH
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6471213/
• Gut Microbiota and Endometriosis – Scientific Reports
https://www.nature.com/articles/s41598-019-39645-2
• How the Gut Influences Hormones – Integrative Medicine Journal
1. The Gut Microbiome: Your Internal Ecosystem
Your gut isn’t just a tube for digesting food. It’s home to trillions of bacteria that:
• Help break down food
• Make key nutrients (like B vitamins)
• Train your immune system
• And — importantly — regulate estrogen levels
This bacterial community is called the gut microbiome, and when it’s healthy and diverse, it supports balanced hormones. But when the microbiome is out of balance — a condition called dysbiosis — problems can arise.
2. Estrobolome: The Gut’s Hormone Filte
Inside the gut, a specific group of bacteria known as the estrobolome helps process estrogen. These bacteria produce enzymes (like beta-glucuronidase) that influence how much estrogen is reabsorbed into the bloodstream versus excreted.
When the estrobolome is overactive or underactive, it can lead to:
• Excess circulating estrogen → linked to endometriosis, fibroids, PMS, and breast tendernes
• Too little estrogen → contributing to mood changes, bone loss, and vaginal dryness
So a disrupted gut can directly amplify hormonal imbalances.
3. Inflammation: The Common Denominator
Both gut dysbiosis and endometriosis are associated with chronic inflammation. When the gut barrier is weakened (a condition sometimes called “leaky gut”), it allows inflammatory molecules to pass into the bloodstream. This triggers an immune response — and in people with endometriosis or PCOS, it can worsen pelvic pain, fatigue, and hormonal chaos.

4. What the Research Says
While this field is still developing, early studies have found:
• Women with endometriosis often have altered gut microbiomes compared to those without the condition. [Study: Ata et al., 2019, Scientific Reports]
• A high-fiber, plant-rich diet may help support a more balanced gut flora and improve estrogen metabolism. [Study: Fuhrman et al., 2004, Journal of Nutrition]
• Some researchers are exploring probiotic therapy as a future tool for managing hormone-related conditions.
5. What Can You Do?
You can’t fully control your hormones — but you can support your gut.
Here are some gut-friendly, hormone-supporting habits:
• Eat more fiber: vegetables, fruits, legumes, and seeds
• Avoid excessive sugar and processed foods
• Include fermented foods: yogurt, kefir, sauerkraut, kimchi
• Consider a probiotic — talk to your provider first
• Manage stress — cortisol (the stress hormone) also affects gut balance
• Support liver detoxification (which works with your gut to clear estrogen): eat cruciferous vegetables like broccoli and cauliflower

Final Thoughts
The gut isn’t just about digestion — it’s a key player in how your body handles hormones, pain, and inflammation.
If you’re struggling with endometriosis, PCOS, or unexplained hormone symptoms, supporting your gut might be an empowering place to start.
Want to Learn More?
Here are some helpful articles and research:
• The Gut Microbiome and Estrogen Metabolism – NIH
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6471213/
• Gut Microbiota and Endometriosis – Scientific Reports
https://www.nature.com/articles/s41598-019-39645-2
• How the Gut Influences Hormones – Integrative Medicine Journal
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
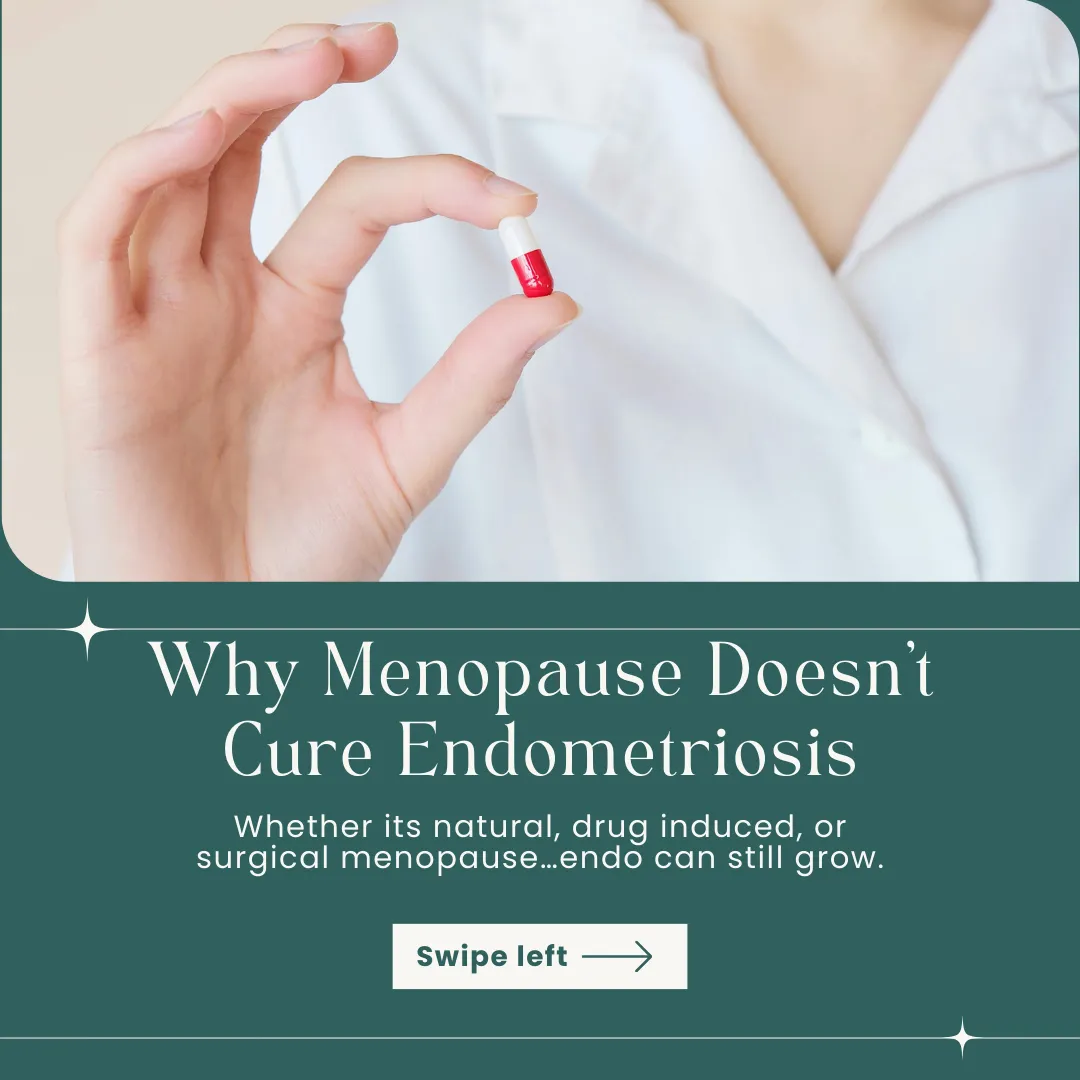
Why Menopause Does Not Treat Endometriosis

Why menopause does not treat endometriosis
Quite often endometriosis patients are told to have their ovaries removed or put their activity on hold with hormonal medication as a way of treating the disease. As demonstrated by some studies, endometriosis lesions have the potential to produce their own oestrogen, as such removal of ovaries or temporary menopause will have little or no impact on the endometriosis itself.
What is oestrogen?
Various laboratory studies have shown that endometriosis is an oestrogen dependent disease. In females, the highest quantity of oestrogens is produced in ovaries. It is also produced in small amounts in other organs such as liver, heart and brain. The oestrogen is divided in three categories: E1 known as estrone, E2 known as estradiol and E3 known as estriol.
Out of all 3 oestrogen types the E2 is the most potent and it is active during the fertility period. E1 is more potent after the menopause and it is synthesised in adipose tissue from adrenal dehydroepiandrosterone, whilst E3 has a role in pregnancy, it’s produced by placenta during pregnancy, and it is the least potent one.
What is aromatase?
The conversion of androstenedione and testosterone E1 and E2 is done by the aromatase. Aromatase is expressed in places such as the brain, gonads, blood vessels, adipose tissue, liver, bone, skin, and endometrium. In fertile women the oestrogen biosynthesis takes place in the ovary, while in postmenopausal women it takes in extraglandular tissues such as adipose tissue and skin.
The role of aromatase expression in endometriosis
One of the first studies that have demonstrated the presence of aromatase expression in endometriosis implants was published in 1996.
To demonstrate the presence of aromatase in endometriosis implants, the scholars have conducted a study analysing and comparing biopsy samples from:
endometriosis implants from pelvic peritoneum (posterior cul-de-sac, bladder, and anterior cul-de-sac);
endometrial tissue in patients with histologically documented pelvic endometriosis;
pelvic peritoneal distal and normal endometrial tissues from women without endometriosis;
Based on the results, P450arom transcripts were detected in all endometriosis implants.The highest presence of P450arom was detected in endometriosis implants that involved the full thickness of the anterior abdominal wall. Also, in the core of the endometriosis implants, the P450arom transcript level was 4-fold higher than that in the surrounding adipose tissue. The authors concluded that the possibility of oestrogen production in endometriosis implants might promote their growth.
Other studies have also demonstrated a higher expression of aromatase in endometriosis implants. Zeitoun KM et al. concluded that molecular aberrations can impact the oestrogen biosynthesis leading to an increased local concentration of E2. The aberrant expressed aromatase in the endometriotic stromal cells converts C19, steroids to oestrogens.
Moreover, a immunohistochemical analysis found that the local estrogen production by aberrantly elevated aromatase takes place only in endometriosis and adenomyosis, and not in the normal endometrium.
In conclusion, removal of ovaries to stop the production of oestrogen as a way of treating endometriosis is not an efficient method, especially if endometriosis lesions are not removed. Endometriosis produces its own oestrogen and as long as the disease is left beyond it will continue to cause symptoms and impact organs.
-Athens Centre for Endometriosis
