Breaking the Silence: Why Endometriosis Took So Long to Be Taken Seriously
—and What’s Finally Changing
For millions of women around the world, the story of endometriosis is one of pain,
dismissal, and delay. But after decades of silence, the tide is beginning to turn.
Breaking the Silence:
Why Endometriosis Took So Long to Be Taken Seriously
—and What’s Finally Changing
For millions of women around the world, the story of endometriosis is one of pain,
dismissal, and delay. But after decades of silence, the tide is beginning to turn.
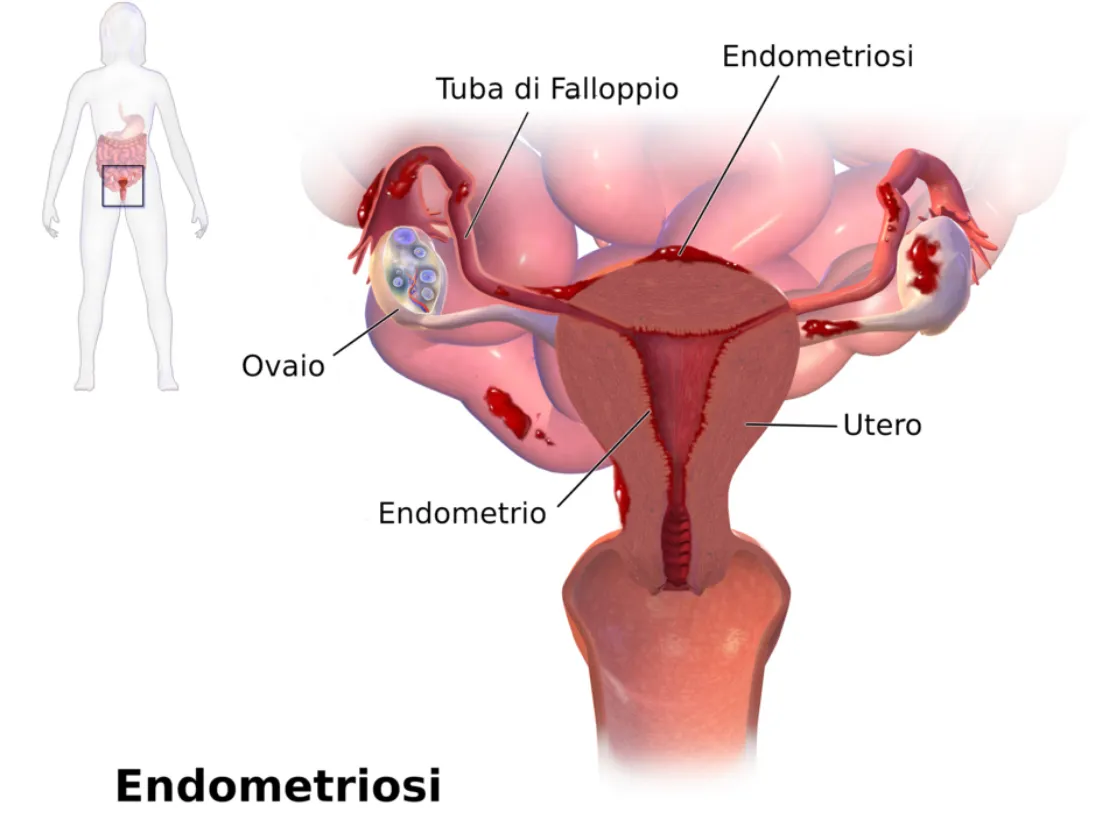
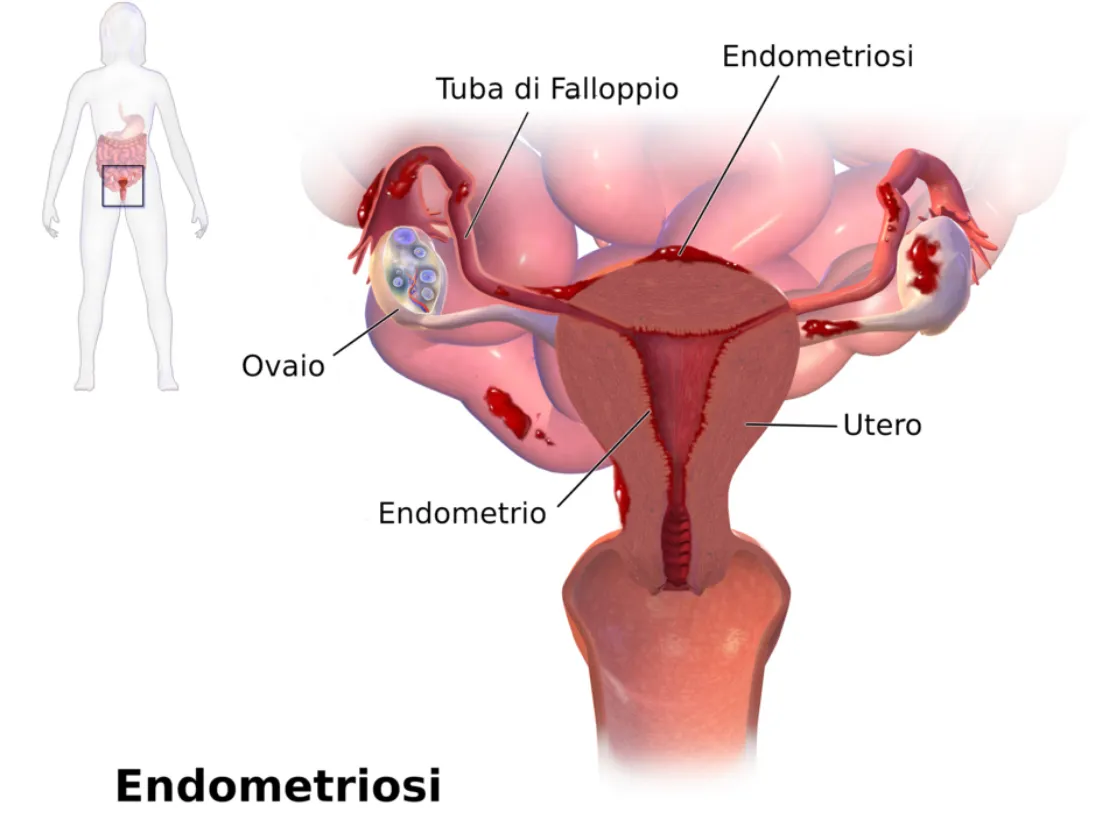
What Is Endometriosis—and Why Has It Been Ignored for So Long
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus grows outside the uterus—on the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond. This tissue responds to hormonal changes, leading to inflammation, scarring, and severe pain.
Despite affecting roughly 1 in 10 women of reproductive age worldwide, endometriosis has historically been misunderstood, underdiagnosed, and mistreated.
World Health Organization Fact Sheet on Endometriosis:
https://www.who.int/news-room/fact-sheets/detail/endometriosis
The Average Time to Diagnosis? Still Over 7 Years.
That’s not a typo. On average, it takes 7 to 10 years from the first symptoms to a correct diagnosis. Why?
• Symptoms are often normalized: Severe period pain? “Just part of being a woman.”
• Lack of non-invasive testing: Diagnosis has long relied on laparoscopic surgery.
• Medical gaps: Many healthcare providers, including OB-GYN’s, receive limited training in gynecologic pain conditions.
NIH: Delays in Endometriosis Diagnosis: https://pubmed.ncbi.nlm.nih.gov/32147966/
What Are the Symptoms of Endometriosis?

Every woman’s experience is different, but some of the most common symptoms include:
• Intense pelvic or abdominal pain
• Pain during or after sex
• Heavy or irregular periods
• Chronic fatigue
• Gastrointestinal issues like bloating, nausea, or constipation
• Infertility or difficulty conceiving
What’s Finally Changing?
Promising Breakthroughs (2024–2025)
New Diagnostic Tools
• MicroRNA panels and blood-based biomarkers are showing promise as non-invasive ways to detect endometriosis earlier.
• Advanced imaging like high-resolution MRI and ultrasound with specialized protocols are helping detect lesions more reliably.
Endometriosis Foundation: Emerging Research: https://www.endofound.org/news-research
PubMed: Biomarkers in Endometriosis: https://pubmed.ncbi.nlm.nih.gov/30807918/
AI & Machine Learning
Artificial intelligence is being trained to analyze symptom patterns, scan images, and even detect potential markers in menstrual blood—offering hope for faster, more accurate screening in the near future.
More Funding and Advocacy
• Governments and nonprofits are increasing research grants.
• Social media and support groups are amplifying women’s voices and experiences.
• Healthcare providers are receiving more training in pelvic pain and minimally invasive surgical options like excision surgery.

What This Means for You (or Someone You Love)
Faster, less invasive diagnosis is on the horizon.
Women are being believed and supported more than ever.
With better understanding comes more targeted treatment options, like hormonal therapies, dietary approaches, pelvic floor therapy, and expert excision surgery.
What You Can Do Right Now
1. Track your symptoms: Keep a daily journal of pain, mood, fatigue, and cycle details.
2. Advocate for yourself: Ask your doctor about excision surgery vs. ablation. A specialist is necessary for proper endometriosis care. Unfortunately, your typical OB-GYN is not an endometriosis or excision specialist.
3. Get support: You're not alone. Online communities and advocacy organizations offer connection and practical help.
Nancy’s Nook Endometriosis Education Group: https://www.facebook.com/groups/NancysNookEndoEd
Center for Endometriosis Care: https://www.centerforendo.com/
Why This Matters
Endometriosis is a whole-body disease that can affect a woman’s physical, emotional, and reproductive health. We are just starting to make some noise & bring attention to this disease and other hormonal diseases related to it.
“The future of women’s health is shifting—but only if we keep raising our voices.”
What Is Endometriosis—and Why Has It Been Ignored for So Long
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus grows outside the uterus—on the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond. This tissue responds to hormonal changes, leading to inflammation, scarring, and severe pain.
Despite affecting roughly 1 in 10 women of reproductive age worldwide, endometriosis has historically been misunderstood, underdiagnosed, and mistreated.
World Health Organization Fact Sheet on Endometriosis:
https://www.who.int/news-room/fact-sheets/detail/endometriosis
The Average Time to Diagnosis? Still Over 7 Years.
That’s not a typo. On average, it takes 7 to 10 years from the first symptoms to a correct diagnosis. Why?
• Symptoms are often normalized: Severe period pain? “Just part of being a woman.”
• Lack of non-invasive testing: Diagnosis has long relied on laparoscopic surgery.
• Medical gaps: Many healthcare providers, including OB-GYN’s, receive limited training in gynecologic pain conditions.
NIH: Delays in Endometriosis Diagnosis: https://pubmed.ncbi.nlm.nih.gov/32147966/
What Are the Symptoms of Endometriosis?

Every woman’s experience is different, but some of the most common symptoms include:
• Intense pelvic or abdominal pain
• Pain during or after sex
• Heavy or irregular periods
• Chronic fatigue
• Gastrointestinal issues like bloating, nausea, or constipation
• Infertility or difficulty conceiving
What’s Finally Changing?
Promising Breakthroughs (2024–2025)
New Diagnostic Tools
• MicroRNA panels and blood-based biomarkers are showing promise as non-invasive ways to detect endometriosis earlier.
• Advanced imaging like high-resolution MRI and ultrasound with specialized protocols are helping detect lesions more reliably.
Endometriosis Foundation: Emerging Research: https://www.endofound.org/news-research
PubMed: Biomarkers in Endometriosis: https://pubmed.ncbi.nlm.nih.gov/30807918/
AI & Machine Learning
Artificial intelligence is being trained to analyze symptom patterns, scan images, and even detect potential markers in menstrual blood—offering hope for faster, more accurate screening in the near future.
More Funding and Advocacy
• Governments and nonprofits are increasing research grants.
• Social media and support groups are amplifying women’s voices and experiences.
• Healthcare providers are receiving more training in pelvic pain and minimally invasive surgical options like excision surgery.

What This Means for You (or Someone You Love)
Faster, less invasive diagnosis is on the horizon.
Women are being believed and supported more than ever.
With better understanding comes more targeted treatment options, like hormonal therapies, dietary approaches, pelvic floor therapy, and expert excision surgery.
What You Can Do Right Now
1. Track your symptoms: Keep a daily journal of pain, mood, fatigue, and cycle details.
2. Advocate for yourself: Ask your doctor about excision surgery vs. ablation. A specialist is necessary for proper endometriosis care. Unfortunately, your typical OB-GYN is not an endometriosis or excision specialist.
3. Get support: You're not alone. Online communities and advocacy organizations offer connection and practical help.
Nancy’s Nook Endometriosis Education Group: https://www.facebook.com/groups/NancysNookEndoEd
Center for Endometriosis Care: https://www.centerforendo.com/
Why This Matters
Endometriosis is a whole-body disease that can affect a woman’s physical, emotional, and reproductive health. We are just starting to make some noise & bring attention to this disease and other hormonal diseases related to it.
“The future of women’s health is shifting—but only if we keep raising our voices.”
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.

My Story: Kathleen Allen

Hi, I’m Kathleen 👋🏻
I’m a mom to three littles and someone who’s walked a long road with women’s health issues—including endometriosis, adenomyosis, ovarian tumors, and a hysterectomy at just 30 years old.
Ever since my first period, I’ve dealt with difficult cycles — heavy bleeding, intense pain, and vomiting that I thought was just “normal.”
After each of my kids, the pain got worse. By my second pregnancy, I was having regular prodromal labor from 20 weeks on, and during my third, it became so severe I ended up having my son prematurely.
After that, the pain stopped following a monthly pattern and started showing up almost every day. I held onto hope for a fourth child, but eventually found out my uterus was in such poor condition from adenomyosis that it was unlikely I could even carry another pregnancy. It was then that I made the difficult decision to have a hysterectomy.
Not long after my hysterectomy, I was referred to an oncologist and was diagnosed with ovarian tumors along with ongoing endometriosis and hormone-related issues. I’ve also dealt with complications from surgery, like perimenopause, adhesions and scar tissue — things many women quietly live with, often without answers. I am currently under the care of the oncology team and expecting to have another surgery in the near future.
These experiences have shaped the path I’m on now. I went back to school to become a functional nutritionist, driven by a deep belief in healing from the inside out. Food and exercise has played a huge role in helping me reclaim my health. I’m committed to living well and helping other women feel empowered in their own health journeys.
I’m sharing this to help bring more awareness to women’s health — because these stories are more common than we think, and they deserve to be talked about.
