Breaking the Silence: Why Endometriosis Took So Long to Be Taken Seriously
—and What’s Finally Changing
For millions of women around the world, the story of endometriosis is one of pain,
dismissal, and delay. But after decades of silence, the tide is beginning to turn.
Breaking the Silence:
Why Endometriosis Took So Long to Be Taken Seriously
—and What’s Finally Changing
For millions of women around the world, the story of endometriosis is one of pain,
dismissal, and delay. But after decades of silence, the tide is beginning to turn.
What Is Endometriosis—and Why Has It Been Ignored for So Long
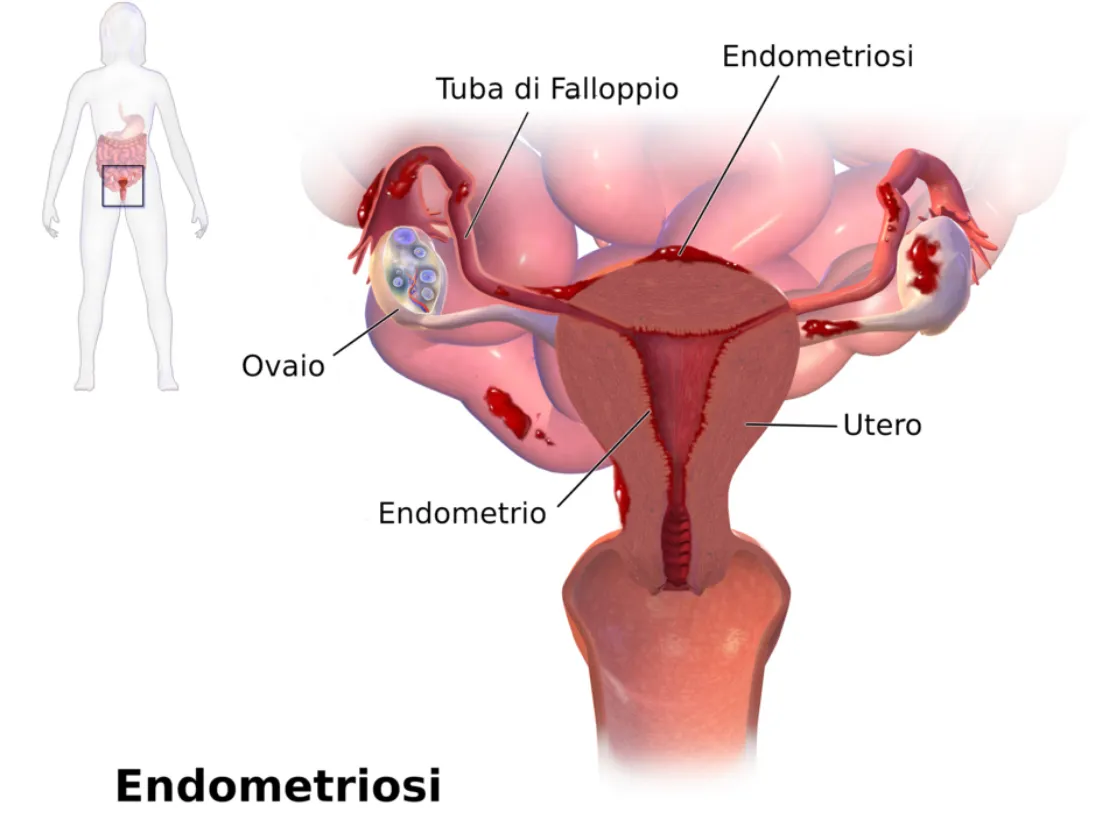
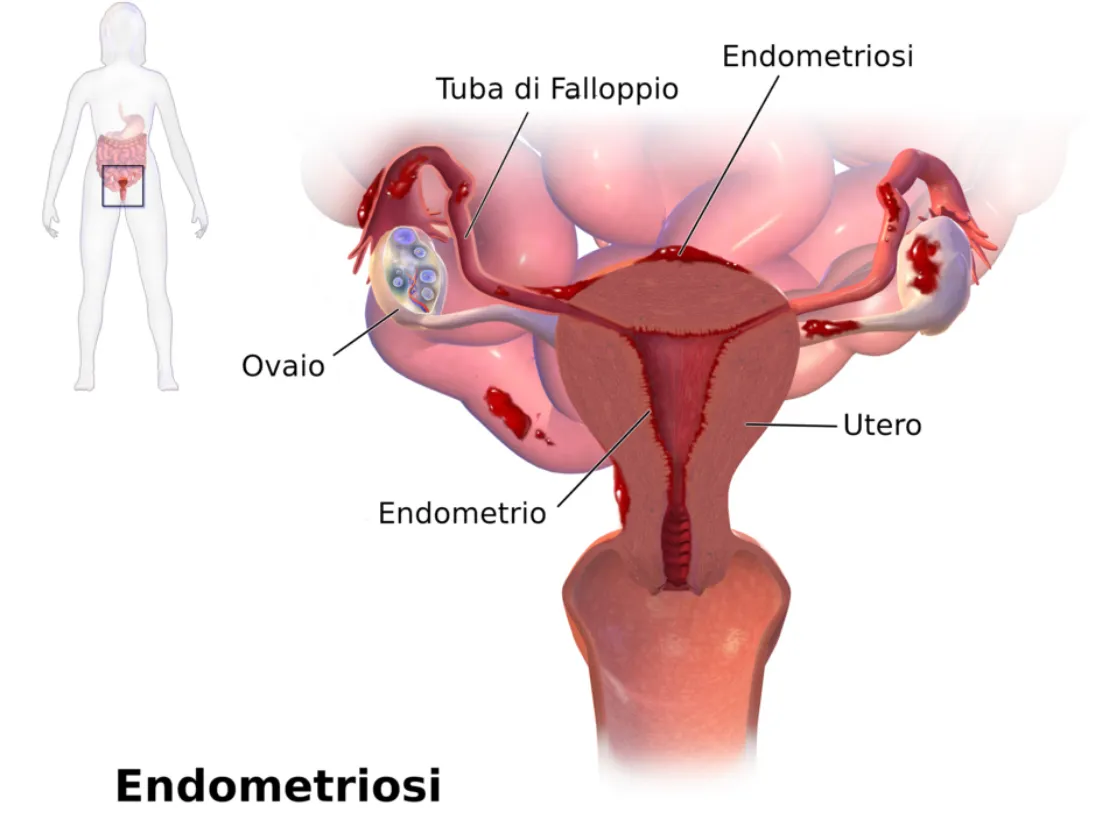
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus grows outside the uterus—on the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond. This tissue responds to hormonal changes, leading to inflammation, scarring, and severe pain.
Despite affecting roughly 1 in 10 women of reproductive age worldwide, endometriosis has historically been misunderstood, underdiagnosed, and mistreated.
World Health Organization Fact Sheet on Endometriosis:
https://www.who.int/news-room/fact-sheets/detail/endometriosis
The Average Time to Diagnosis? Still Over 7 Years.
That’s not a typo. On average, it takes 7 to 10 years from the first symptoms to a correct diagnosis. Why?
• Symptoms are often normalized: Severe period pain? “Just part of being a woman.”
• Lack of non-invasive testing: Diagnosis has long relied on laparoscopic surgery.
• Medical gaps: Many healthcare providers, including OB-GYN’s, receive limited training in gynecologic pain conditions.
NIH: Delays in Endometriosis Diagnosis: https://pubmed.ncbi.nlm.nih.gov/32147966/
What Are the Symptoms of Endometriosis?

Every woman’s experience is different, but some of the most common symptoms include:
• Intense pelvic or abdominal pain
• Pain during or after sex
• Heavy or irregular periods
• Chronic fatigue
• Gastrointestinal issues like bloating, nausea, or constipation
• Infertility or difficulty conceiving
What’s Finally Changing?
Promising Breakthroughs (2024–2025)
New Diagnostic Tools
• MicroRNA panels and blood-based biomarkers are showing promise as non-invasive ways to detect endometriosis earlier.
• Advanced imaging like high-resolution MRI and ultrasound with specialized protocols are helping detect lesions more reliably.
Endometriosis Foundation: Emerging Research: https://www.endofound.org/news-research
PubMed: Biomarkers in Endometriosis: https://pubmed.ncbi.nlm.nih.gov/30807918/
AI & Machine Learning
Artificial intelligence is being trained to analyze symptom patterns, scan images, and even detect potential markers in menstrual blood—offering hope for faster, more accurate screening in the near future.
More Funding and Advocacy
• Governments and nonprofits are increasing research grants.
• Social media and support groups are amplifying women’s voices and experiences.
• Healthcare providers are receiving more training in pelvic pain and minimally invasive surgical options like excision surgery.

What This Means for You (or Someone You Love)
Faster, less invasive diagnosis is on the horizon.
Women are being believed and supported more than ever.
With better understanding comes more targeted treatment options, like hormonal therapies, dietary approaches, pelvic floor therapy, and expert excision surgery.
What You Can Do Right Now
1. Track your symptoms: Keep a daily journal of pain, mood, fatigue, and cycle details.
2. Advocate for yourself: Ask your doctor about excision surgery vs. ablation. A specialist is necessary for proper endometriosis care. Unfortunately, your typical OB-GYN is not an endometriosis or excision specialist.
3. Get support: You're not alone. Online communities and advocacy organizations offer connection and practical help.
Nancy’s Nook Endometriosis Education Group: https://www.facebook.com/groups/NancysNookEndoEd
Center for Endometriosis Care: https://www.centerforendo.com/
Why This Matters
Endometriosis is a whole-body disease that can affect a woman’s physical, emotional, and reproductive health. We are just starting to make some noise & bring attention to this disease and other hormonal diseases related to it.
“The future of women’s health is shifting—but only if we keep raising our voices.”
What Is Endometriosis—and Why Has It Been Ignored for So Long
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus grows outside the uterus—on the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond. This tissue responds to hormonal changes, leading to inflammation, scarring, and severe pain.
Despite affecting roughly 1 in 10 women of reproductive age worldwide, endometriosis has historically been misunderstood, underdiagnosed, and mistreated.
World Health Organization Fact Sheet on Endometriosis:
https://www.who.int/news-room/fact-sheets/detail/endometriosis
The Average Time to Diagnosis? Still Over 7 Years.
That’s not a typo. On average, it takes 7 to 10 years from the first symptoms to a correct diagnosis. Why?
• Symptoms are often normalized: Severe period pain? “Just part of being a woman.”
• Lack of non-invasive testing: Diagnosis has long relied on laparoscopic surgery.
• Medical gaps: Many healthcare providers, including OB-GYN’s, receive limited training in gynecologic pain conditions.
NIH: Delays in Endometriosis Diagnosis: https://pubmed.ncbi.nlm.nih.gov/32147966/
What Are the Symptoms of Endometriosis?

Every woman’s experience is different, but some of the most common symptoms include:
• Intense pelvic or abdominal pain
• Pain during or after sex
• Heavy or irregular periods
• Chronic fatigue
• Gastrointestinal issues like bloating, nausea, or constipation
• Infertility or difficulty conceiving
What’s Finally Changing?
Promising Breakthroughs (2024–2025)
New Diagnostic Tools
• MicroRNA panels and blood-based biomarkers are showing promise as non-invasive ways to detect endometriosis earlier.
• Advanced imaging like high-resolution MRI and ultrasound with specialized protocols are helping detect lesions more reliably.
Endometriosis Foundation: Emerging Research: https://www.endofound.org/news-research
PubMed: Biomarkers in Endometriosis: https://pubmed.ncbi.nlm.nih.gov/30807918/
AI & Machine Learning
Artificial intelligence is being trained to analyze symptom patterns, scan images, and even detect potential markers in menstrual blood—offering hope for faster, more accurate screening in the near future.
More Funding and Advocacy
• Governments and nonprofits are increasing research grants.
• Social media and support groups are amplifying women’s voices and experiences.
• Healthcare providers are receiving more training in pelvic pain and minimally invasive surgical options like excision surgery.

What This Means for You (or Someone You Love)
Faster, less invasive diagnosis is on the horizon.
Women are being believed and supported more than ever.
With better understanding comes more targeted treatment options, like hormonal therapies, dietary approaches, pelvic floor therapy, and expert excision surgery.
What You Can Do Right Now
1. Track your symptoms: Keep a daily journal of pain, mood, fatigue, and cycle details.
2. Advocate for yourself: Ask your doctor about excision surgery vs. ablation. A specialist is necessary for proper endometriosis care. Unfortunately, your typical OB-GYN is not an endometriosis or excision specialist.
3. Get support: You're not alone. Online communities and advocacy organizations offer connection and practical help.
Nancy’s Nook Endometriosis Education Group: https://www.facebook.com/groups/NancysNookEndoEd
Center for Endometriosis Care: https://www.centerforendo.com/
Why This Matters
Endometriosis is a whole-body disease that can affect a woman’s physical, emotional, and reproductive health. We are just starting to make some noise & bring attention to this disease and other hormonal diseases related to it.
“The future of women’s health is shifting—but only if we keep raising our voices.”
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.

Relaxing Your Pelvic Floor
Relaxing the Pelvic Floor: Simple Practices with Powerful Benefits
Tension in the pelvic floor is more common than many realize—and it can be a significant source of pain, dysfunction, and stress. While most people have heard of Kegels to strengthen pelvic floor muscles, the equally important skill of relaxing those muscles is often overlooked. Chronic tightness in the pelvic floor can lead to a range of symptoms including pelvic pain, urinary urgency, painful intercourse, constipation, and low back pain.
*Your pelvic floor carries a lot—physically and emotionally. Incorporating simple tools like these into your daily routine isn’t just about relief after symptoms hit—it’s about building a system that might help prevent them before they start. A few minutes of deep breathing, gentle movement, or a warm bath can help calm your nervous system, ease tension, and support your body.That said, flare-ups aren’t always in your control—and that doesn’t mean you’re doing anything wrong. This is the nature of endometriosis. These are just supportive tools, not a cure—but sometimes, little things can make a big difference.
Fortunately, simple daily techniques—like the ones illustrated by @beyondbasicspt in the graphic above—can make a profound difference. Let’s break down each method and explore what the research says.
1. Deep Belly Breathing with Humming
Slow diaphragmatic breathing encourages the pelvic floor to relax naturally. When you inhale deeply, your diaphragm moves downward, and this movement is mirrored by the pelvic floor, creating a gentle stretch and release.
Why add humming? Humming stimulates the vagus nerve, which activates the parasympathetic nervous system (the “rest and digest” response), helping the entire pelvic region soften.
Research Insight: A 2020 study published in Pain Medicine found that slow, diaphragmatic breathing improved outcomes in patients with chronic pelvic pain by reducing muscle tone and improving nervous system regulation (Mehling et al., 2020).
2. Warm Bath
Immersion in warm water increases blood flow and reduces muscle guarding—especially in the pelvic area. The buoyancy also helps reduce gravitational compression, encouraging muscle relaxation.
Research Insight: Hydrotherapy has long been shown to reduce muscle tension and improve circulation (Kamioka et al., 2010). For pelvic pain specifically, warmth and hydrostatic pressure may help ease myofascial tension in the pelvic floor.
3. Pelvic Floor Drop (Let-Go Technique)
Unlike Kegels (which focus on contraction), the pelvic floor drop emphasizes releasing and lengthening the pelvic muscles. Think of it as the "exhale and let go" moment for the pelvic floor.
Research Insight: A 2016 review in the Journal of Bodywork and Movement Therapies emphasizes that relaxation techniques—including conscious "letting go"—are key in treating non-relaxing pelvic floor dysfunction (FitzGerald et al., 2016).
4. Gentle Hip Circles
These rhythmic movements help mobilize the hips and pelvis, gently loosening fascia and improving circulation in the pelvic region.
Research Insight: Movement therapies that increase pelvic mobility are beneficial in reducing hypertonicity (muscle overactivity) in the pelvic floor (Haugstad et al., 2006).
5. Legs-Up-The-Wall Pose
Known as Viparita Karani in yoga, this pose promotes venous return and encourages full-body relaxation. It also reduces pressure in the pelvic region and helps calm the nervous system.
Research Insight: A 2013 study in Evidence-Based Complementary and Alternative Medicine noted that restorative yoga poses, like legs-up-the-wall, reduce sympathetic nervous system activity and improve muscle tone regulation (Telles et al., 2013).
6. Jaw + Neck Massage
Here’s a fascinating link: the jaw and the pelvic floor are neurologically and developmentally connected. Tension in one area often reflects or reinforces tension in the other.
Tip: Try gently massaging the base of your skull and jawline—or even releasing your tongue from the roof of your mouth—to help the pelvic muscles relax.
Research Insight: Somatic connections between the jaw and pelvis have been observed in body-oriented therapies. A 2021 review published in Medical Hypotheses proposed shared motor control pathways that link craniofacial and pelvic floor muscle groups (Wallden, 2021).
Final Thoughts
Pelvic floor relaxation isn’t just about relieving pain—it’s about restoring balance, function, and a sense of ease in the body. Whether you’re dealing with pelvic pain, recovering from childbirth, or simply seeking more mind-body awareness, these gentle practices are worth integrating into your daily routine.
As always, if you're experiencing persistent pelvic discomfort, consult a pelvic floor physical therapist for a personalized plan. These professionals can guide you through both strengthening and relaxation techniques safely.
References
Mehling, W. E., et al. (2020). Effects of breathing retraining on chronic pelvic pain. Pain Medicine, 21(4), 798–808.
Kamioka, H., et al. (2010). Effectiveness of aquatic exercise and balneotherapy: A summary of systematic reviews. Journal of Epidemiology, 20(1), 2–12.
FitzGerald, M. P., et al. (2016). Evaluation and treatment of non-relaxing pelvic floor dysfunction. J Bodyw Mov Ther, 20(2), 275–281.
Haugstad, G. K., et al. (2006). Muscular and non-muscular responses to movement therapy in women with chronic pelvic pain. Physiotherapy Research International, 11(4), 217–228.
Telles, S., et al. (2013). Restorative yoga for women with pelvic pain: a randomized controlled trial. Evid Based Complement Alternat Med, 2013, 792581.
Wallden, M. (2021). The anatomical and neurobiological link between the jaw and pelvic floor. Medical Hypotheses, 150, 110556.
