Breaking the Silence: Why Endometriosis Took So Long to Be Taken Seriously
—and What’s Finally Changing
For millions of women around the world, the story of endometriosis is one of pain,
dismissal, and delay. But after decades of silence, the tide is beginning to turn.
Breaking the Silence:
Why Endometriosis Took So Long to Be Taken Seriously
—and What’s Finally Changing
For millions of women around the world, the story of endometriosis is one of pain,
dismissal, and delay. But after decades of silence, the tide is beginning to turn.
What Is Endometriosis—and Why Has It Been Ignored for So Long
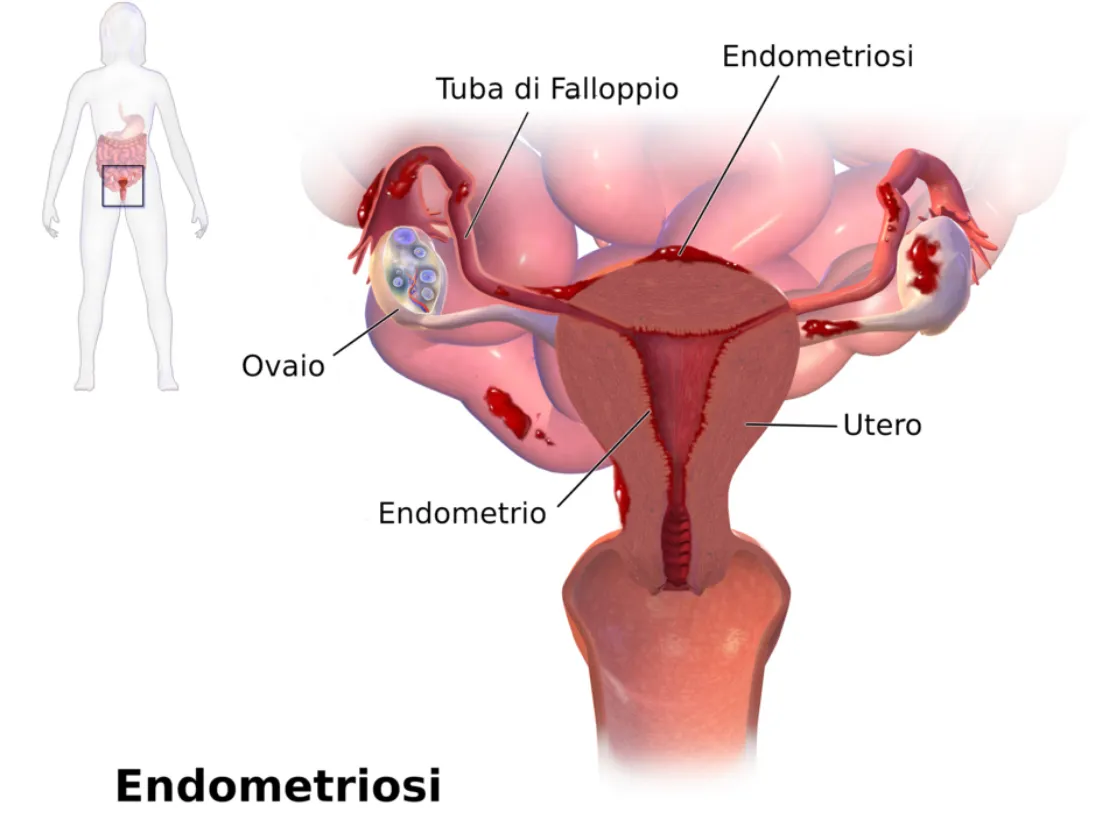
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus grows outside the uterus—on the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond. This tissue responds to hormonal changes, leading to inflammation, scarring, and severe pain.
Despite affecting roughly 1 in 10 women of reproductive age worldwide, endometriosis has historically been misunderstood, underdiagnosed, and mistreated.
World Health Organization Fact Sheet on Endometriosis:
https://www.who.int/news-room/fact-sheets/detail/endometriosis
The Average Time to Diagnosis? Still Over 7 Years.
That’s not a typo. On average, it takes 7 to 10 years from the first symptoms to a correct diagnosis. Why?
• Symptoms are often normalized: Severe period pain? “Just part of being a woman.”
• Lack of non-invasive testing: Diagnosis has long relied on laparoscopic surgery.
• Medical gaps: Many healthcare providers, including OB-GYN’s, receive limited training in gynecologic pain conditions.
NIH: Delays in Endometriosis Diagnosis: https://pubmed.ncbi.nlm.nih.gov/32147966/
What Are the Symptoms of Endometriosis?

Every woman’s experience is different, but some of the most common symptoms include:
• Intense pelvic or abdominal pain
• Pain during or after sex
• Heavy or irregular periods
• Chronic fatigue
• Gastrointestinal issues like bloating, nausea, or constipation
• Infertility or difficulty conceiving
What’s Finally Changing?
Promising Breakthroughs (2024–2025)
New Diagnostic Tools
• MicroRNA panels and blood-based biomarkers are showing promise as non-invasive ways to detect endometriosis earlier.
• Advanced imaging like high-resolution MRI and ultrasound with specialized protocols are helping detect lesions more reliably.
Endometriosis Foundation: Emerging Research: https://www.endofound.org/news-research
PubMed: Biomarkers in Endometriosis: https://pubmed.ncbi.nlm.nih.gov/30807918/
AI & Machine Learning
Artificial intelligence is being trained to analyze symptom patterns, scan images, and even detect potential markers in menstrual blood—offering hope for faster, more accurate screening in the near future.
More Funding and Advocacy
• Governments and nonprofits are increasing research grants.
• Social media and support groups are amplifying women’s voices and experiences.
• Healthcare providers are receiving more training in pelvic pain and minimally invasive surgical options like excision surgery.

What This Means for You (or Someone You Love)
Faster, less invasive diagnosis is on the horizon.
Women are being believed and supported more than ever.
With better understanding comes more targeted treatment options, like hormonal therapies, dietary approaches, pelvic floor therapy, and expert excision surgery.
What You Can Do Right Now
1. Track your symptoms: Keep a daily journal of pain, mood, fatigue, and cycle details.
2. Advocate for yourself: Ask your doctor about excision surgery vs. ablation. A specialist is necessary for proper endometriosis care. Unfortunately, your typical OB-GYN is not an endometriosis or excision specialist.
3. Get support: You're not alone. Online communities and advocacy organizations offer connection and practical help.
Nancy’s Nook Endometriosis Education Group: https://www.facebook.com/groups/NancysNookEndoEd
Center for Endometriosis Care: https://www.centerforendo.com/
Why This Matters
Endometriosis is a whole-body disease that can affect a woman’s physical, emotional, and reproductive health. We are just starting to make some noise & bring attention to this disease and other hormonal diseases related to it.
“The future of women’s health is shifting—but only if we keep raising our voices.”
What Is Endometriosis—and Why Has It Been Ignored for So Long
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus grows outside the uterus—on the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond. This tissue responds to hormonal changes, leading to inflammation, scarring, and severe pain.
Despite affecting roughly 1 in 10 women of reproductive age worldwide, endometriosis has historically been misunderstood, underdiagnosed, and mistreated.
World Health Organization Fact Sheet on Endometriosis:
https://www.who.int/news-room/fact-sheets/detail/endometriosis
The Average Time to Diagnosis? Still Over 7 Years.
That’s not a typo. On average, it takes 7 to 10 years from the first symptoms to a correct diagnosis. Why?
• Symptoms are often normalized: Severe period pain? “Just part of being a woman.”
• Lack of non-invasive testing: Diagnosis has long relied on laparoscopic surgery.
• Medical gaps: Many healthcare providers, including OB-GYN’s, receive limited training in gynecologic pain conditions.
NIH: Delays in Endometriosis Diagnosis: https://pubmed.ncbi.nlm.nih.gov/32147966/
What Are the Symptoms of Endometriosis?

Every woman’s experience is different, but some of the most common symptoms include:
• Intense pelvic or abdominal pain
• Pain during or after sex
• Heavy or irregular periods
• Chronic fatigue
• Gastrointestinal issues like bloating, nausea, or constipation
• Infertility or difficulty conceiving
What’s Finally Changing?
Promising Breakthroughs (2024–2025)
New Diagnostic Tools
• MicroRNA panels and blood-based biomarkers are showing promise as non-invasive ways to detect endometriosis earlier.
• Advanced imaging like high-resolution MRI and ultrasound with specialized protocols are helping detect lesions more reliably.
Endometriosis Foundation: Emerging Research: https://www.endofound.org/news-research
PubMed: Biomarkers in Endometriosis: https://pubmed.ncbi.nlm.nih.gov/30807918/
AI & Machine Learning
Artificial intelligence is being trained to analyze symptom patterns, scan images, and even detect potential markers in menstrual blood—offering hope for faster, more accurate screening in the near future.
More Funding and Advocacy
• Governments and nonprofits are increasing research grants.
• Social media and support groups are amplifying women’s voices and experiences.
• Healthcare providers are receiving more training in pelvic pain and minimally invasive surgical options like excision surgery.

What This Means for You (or Someone You Love)
Faster, less invasive diagnosis is on the horizon.
Women are being believed and supported more than ever.
With better understanding comes more targeted treatment options, like hormonal therapies, dietary approaches, pelvic floor therapy, and expert excision surgery.
What You Can Do Right Now
1. Track your symptoms: Keep a daily journal of pain, mood, fatigue, and cycle details.
2. Advocate for yourself: Ask your doctor about excision surgery vs. ablation. A specialist is necessary for proper endometriosis care. Unfortunately, your typical OB-GYN is not an endometriosis or excision specialist.
3. Get support: You're not alone. Online communities and advocacy organizations offer connection and practical help.
Nancy’s Nook Endometriosis Education Group: https://www.facebook.com/groups/NancysNookEndoEd
Center for Endometriosis Care: https://www.centerforendo.com/
Why This Matters
Endometriosis is a whole-body disease that can affect a woman’s physical, emotional, and reproductive health. We are just starting to make some noise & bring attention to this disease and other hormonal diseases related to it.
“The future of women’s health is shifting—but only if we keep raising our voices.”
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
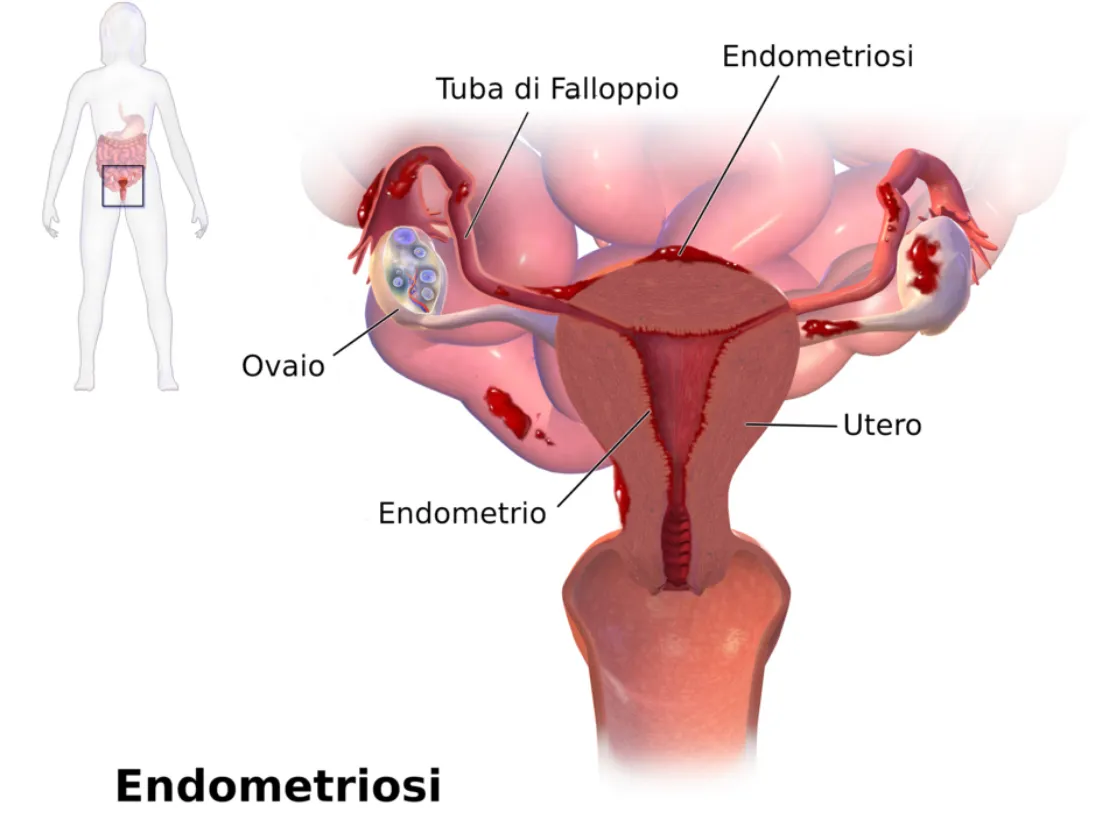
Neuroangiogenesis: Nerves & Blood Vessels Fueling Endo
How Nerves and Blood Vessels Fuel Endometriosis: Understanding Neuroangiogenesis
When we think of endometriosis, we often imagine painful periods, reproductive complications, or fatigue. But beneath these symptoms lies a deeper, more complex process—one that helps explain why this condition is so painful, why it often gets worse over time, and why standard treatments don’t always work.
That process is called neuroangiogenesis—a mouthful of a word that simply means the simultaneous growth of new nerves (neuro-) and blood vessels (-angiogenesis). And it’s changing the way experts understand and treat endometriosis.
What Is Neuroangiogenesis?
Dr. Vimee Bindra, a leading gynecologist and endometriosis specialist, puts it plainly:
“Neuroangiogenesis fuels the pain of endometriosis.”
In her article, she explains that endometriotic lesions aren’t passive—they actively create their own support systems. These lesions grow tiny blood vessels that bring in oxygen and nutrients, helping them survive even in hostile environments like the pelvis, bowel, bladder, or abdominal wall. But even more troubling, they also stimulate nerve growth—making the affected areas more sensitive and painful.
This explains why pain in endometriosis isn’t limited to menstruation. For many women, it’s constant. It flares during ovulation. It radiates into the legs or back. It worsens with movement, digestion, or intimacy.
Why? Because it’s not just inflammation—it’s nerve-driven pain. The same biological mechanisms that help our body heal after injury are being hijacked by endometriosis lesions to sustain and spread the disease.
The Science Behind It
Research supports this dual growth model:
Studies have found that vascular endothelial growth factor (VEGF), which encourages new blood vessel formation, is overproduced in endometriotic tissue.
At the same time, nerve growth factor (NGF) is elevated, helping lesions become densely innervated and hypersensitive.
In fact, some studies report that lesions have 10 to 50 times more nerve fibers than similar tissue in people without endometriosis.
This combination of angiogenesis and neurogenesis makes endometriosis uniquely painful—and uniquely difficult to treat with one-size-fits-all approaches.
Why It Matters
Pain is not just a symptom of endometriosis—it’s a sign of progression.
Neuroangiogenesis helps explain why:
Endometriosis pain doesn’t always correlate with the size of lesions.
Pain can continue even after menopause or a hysterectomy.
Hormonal treatments alone often fail to fully relieve symptoms.
Dr. Bindra emphasizes that neuroangiogenesis helps us reframe endometriosis not just as a hormonal or reproductive issue, but as a neurovascular condition—one that affects the immune system, the nervous system, and the vascular system all at once.
Understanding this has the potential to unlock better, longer-lasting solutions.
A New Direction for Treatment
This evolving science is already inspiring a shift in how endometriosis is treated:
1. Anti-Angiogenic Therapies
By targeting VEGF and other blood vessel growth signals, researchers hope to “starve” lesions and stop them from spreading. Some cancer drugs are being investigated for this purpose, including bevacizumab, which blocks VEGF.
2. Nerve-Targeted Treatments
Medications that calm overactive nerves—such as gabapentin, pregabalin, or even newer biologics aimed at NGF—may help reduce pain at its neurological source.
3. Precision Surgery
Excision surgery done by skilled specialists—especially when guided by lesion-mapping tools like the ENZIAN classification—can remove deep, infiltrating lesions and decompress trapped nerves. This type of surgery is different from ablation and requires specialized expertise, but it can offer significant relief.
As Dr. Bindra notes in her clinical work, identifying the exact location and depth of lesions—especially those invading nerves—is critical for improving surgical outcomes.
Hope on the Horizon
At Our Daughters Foundation, we believe that informed care is empowered care. And understanding neuroangiogenesis gives us all a better framework for navigating endometriosis.
It helps patients explain their pain.
It helps doctors pursue more targeted treatments.
And it helps researchers continue moving toward real, long-term solutions.
You are not imagining your pain. You are not overreacting. You are not alone.
“The more we learn about how endometriosis builds its own nerve and blood supply, the closer we get to stopping it at the source.” – Dr. Vimee Bindra
References
Dr. Vimee Bindra
“Neuroangiogenesis: How Nerves and Blood Vessels Fuel Endometriosis”
https://www.drvimeebindra.com/neuroangiogenesis-how-nerves-and-blood-vessels-fuel-endometriosis/Dr. Vimee Bindra (LinkedIn)
Quote: “Neuroangiogenesis fuels the pain of endometriosis…”
https://www.linkedin.com/posts/dr-vimee-bindra-basu-7514765b_letstalkendo-endometriosisawarenessmonth-activity-7305270488694501381-KtCYTokushige N, Markham R, Russell P, Fraser IS
“Nerve fibers in peritoneal endometriosis”
Human Reproduction, 2006.
https://doi.org/10.1093/humrep/del009Taylor RN, Yu J, Torres PB, Schickedanz AC, Park JK, Mueller MD
“Mechanistic and therapeutic implications of angiogenesis in endometriosis”
Reproductive Sciences, 2020.
https://doi.org/10.1177/1933719119899937Arnold J, Barcena de Arellano ML, Rüster C, et al.
“Immunologic alterations in endometriosis: current understanding and future therapeutic implications”
Journal of Clinical Medicine, 2020.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7349441/Ferrero S, Gillott DJ, Remorgida V, et al.
“Use of antiangiogenic agents to treat endometriosis: a review”
Gynecological Endocrinology, 2010.
https://doi.org/10.3109/09513590903247814Bindra V, et al.
“Clinical Characteristics and Locations of Lesions in Patients with Endometriosis Using ENZIAN Classification”
Journal of Obstetrics and Gynaecology of India, 2025.
https://pubmed.ncbi.nlm.nih.gov/40390882/
