Breaking the Silence: Why Endometriosis Took So Long to Be Taken Seriously
—and What’s Finally Changing
For millions of women around the world, the story of endometriosis is one of pain,
dismissal, and delay. But after decades of silence, the tide is beginning to turn.
Breaking the Silence:
Why Endometriosis Took So Long to Be Taken Seriously
—and What’s Finally Changing
For millions of women around the world, the story of endometriosis is one of pain,
dismissal, and delay. But after decades of silence, the tide is beginning to turn.
What Is Endometriosis—and Why Has It Been Ignored for So Long
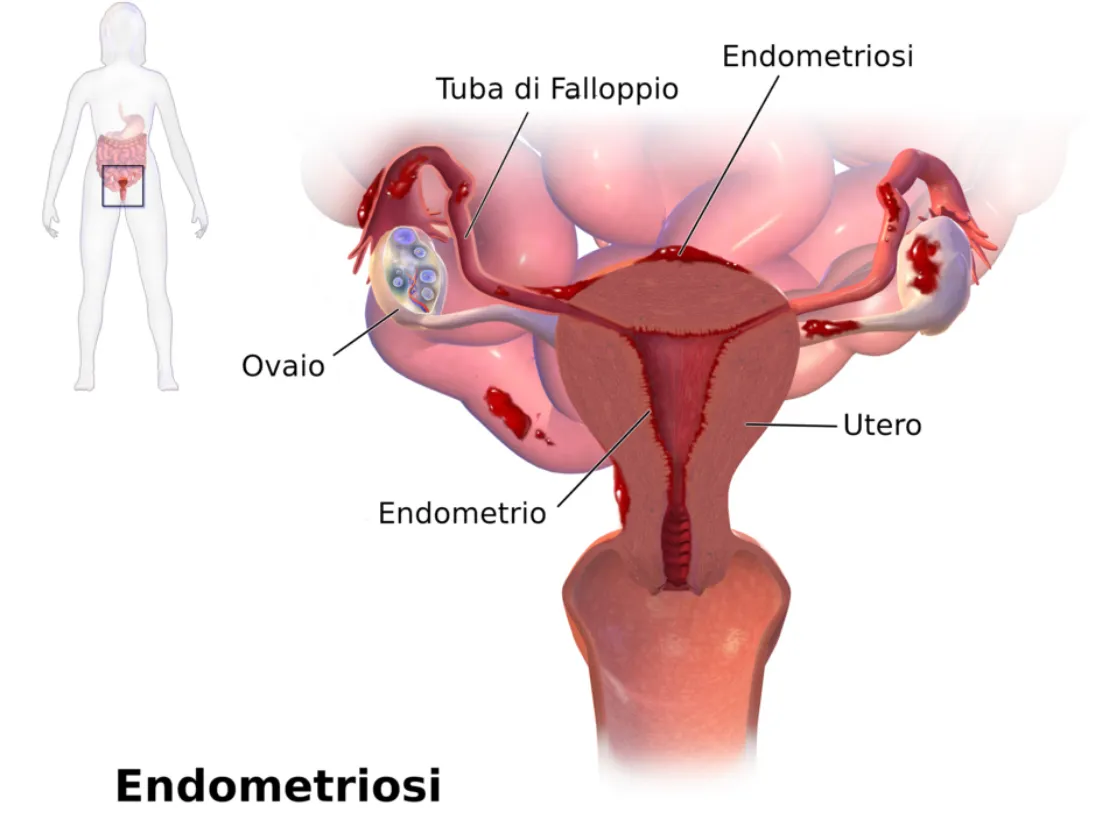
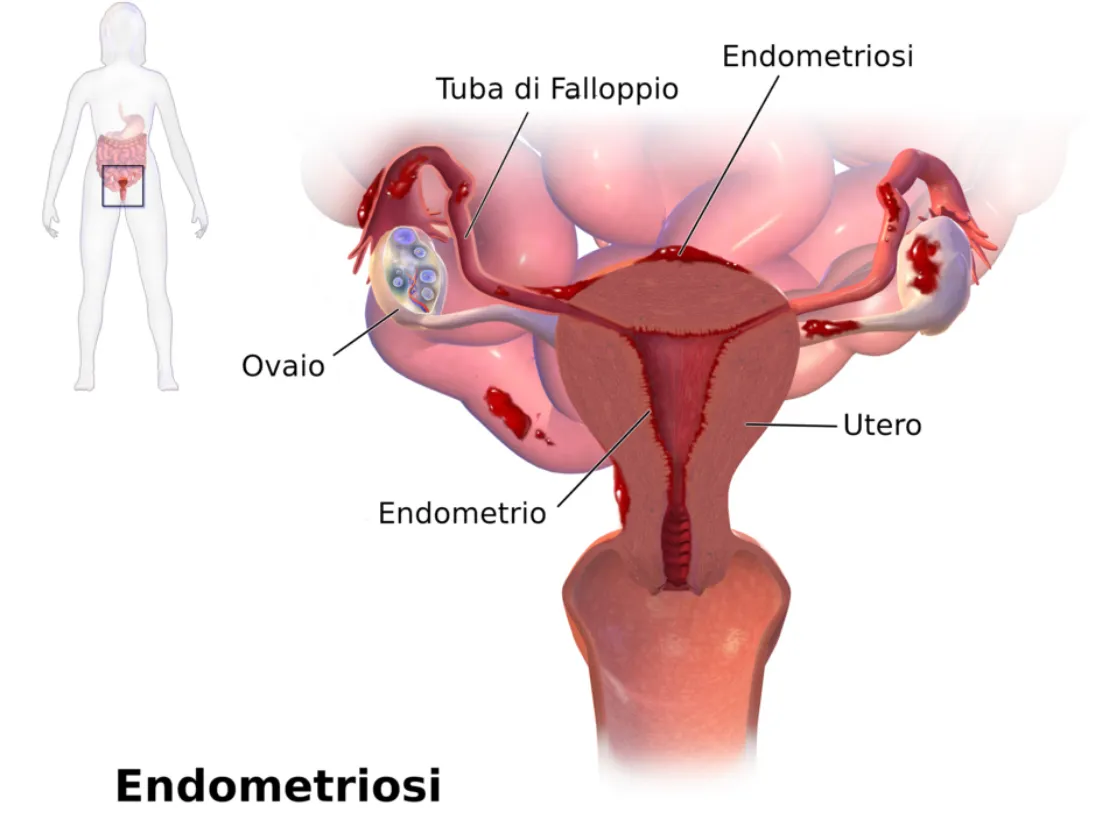
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus grows outside the uterus—on the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond. This tissue responds to hormonal changes, leading to inflammation, scarring, and severe pain.
Despite affecting roughly 1 in 10 women of reproductive age worldwide, endometriosis has historically been misunderstood, underdiagnosed, and mistreated.
World Health Organization Fact Sheet on Endometriosis:
https://www.who.int/news-room/fact-sheets/detail/endometriosis
The Average Time to Diagnosis? Still Over 7 Years.
That’s not a typo. On average, it takes 7 to 10 years from the first symptoms to a correct diagnosis. Why?
• Symptoms are often normalized: Severe period pain? “Just part of being a woman.”
• Lack of non-invasive testing: Diagnosis has long relied on laparoscopic surgery.
• Medical gaps: Many healthcare providers, including OB-GYN’s, receive limited training in gynecologic pain conditions.
NIH: Delays in Endometriosis Diagnosis: https://pubmed.ncbi.nlm.nih.gov/32147966/
What Are the Symptoms of Endometriosis?

Every woman’s experience is different, but some of the most common symptoms include:
• Intense pelvic or abdominal pain
• Pain during or after sex
• Heavy or irregular periods
• Chronic fatigue
• Gastrointestinal issues like bloating, nausea, or constipation
• Infertility or difficulty conceiving
What’s Finally Changing?
Promising Breakthroughs (2024–2025)
New Diagnostic Tools
• MicroRNA panels and blood-based biomarkers are showing promise as non-invasive ways to detect endometriosis earlier.
• Advanced imaging like high-resolution MRI and ultrasound with specialized protocols are helping detect lesions more reliably.
Endometriosis Foundation: Emerging Research: https://www.endofound.org/news-research
PubMed: Biomarkers in Endometriosis: https://pubmed.ncbi.nlm.nih.gov/30807918/
AI & Machine Learning
Artificial intelligence is being trained to analyze symptom patterns, scan images, and even detect potential markers in menstrual blood—offering hope for faster, more accurate screening in the near future.
More Funding and Advocacy
• Governments and nonprofits are increasing research grants.
• Social media and support groups are amplifying women’s voices and experiences.
• Healthcare providers are receiving more training in pelvic pain and minimally invasive surgical options like excision surgery.

What This Means for You (or Someone You Love)
Faster, less invasive diagnosis is on the horizon.
Women are being believed and supported more than ever.
With better understanding comes more targeted treatment options, like hormonal therapies, dietary approaches, pelvic floor therapy, and expert excision surgery.
What You Can Do Right Now
1. Track your symptoms: Keep a daily journal of pain, mood, fatigue, and cycle details.
2. Advocate for yourself: Ask your doctor about excision surgery vs. ablation. A specialist is necessary for proper endometriosis care. Unfortunately, your typical OB-GYN is not an endometriosis or excision specialist.
3. Get support: You're not alone. Online communities and advocacy organizations offer connection and practical help.
Nancy’s Nook Endometriosis Education Group: https://www.facebook.com/groups/NancysNookEndoEd
Center for Endometriosis Care: https://www.centerforendo.com/
Why This Matters
Endometriosis is a whole-body disease that can affect a woman’s physical, emotional, and reproductive health. We are just starting to make some noise & bring attention to this disease and other hormonal diseases related to it.
“The future of women’s health is shifting—but only if we keep raising our voices.”
What Is Endometriosis—and Why Has It Been Ignored for So Long
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus grows outside the uterus—on the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond. This tissue responds to hormonal changes, leading to inflammation, scarring, and severe pain.
Despite affecting roughly 1 in 10 women of reproductive age worldwide, endometriosis has historically been misunderstood, underdiagnosed, and mistreated.
World Health Organization Fact Sheet on Endometriosis:
https://www.who.int/news-room/fact-sheets/detail/endometriosis
The Average Time to Diagnosis? Still Over 7 Years.
That’s not a typo. On average, it takes 7 to 10 years from the first symptoms to a correct diagnosis. Why?
• Symptoms are often normalized: Severe period pain? “Just part of being a woman.”
• Lack of non-invasive testing: Diagnosis has long relied on laparoscopic surgery.
• Medical gaps: Many healthcare providers, including OB-GYN’s, receive limited training in gynecologic pain conditions.
NIH: Delays in Endometriosis Diagnosis: https://pubmed.ncbi.nlm.nih.gov/32147966/
What Are the Symptoms of Endometriosis?

Every woman’s experience is different, but some of the most common symptoms include:
• Intense pelvic or abdominal pain
• Pain during or after sex
• Heavy or irregular periods
• Chronic fatigue
• Gastrointestinal issues like bloating, nausea, or constipation
• Infertility or difficulty conceiving
What’s Finally Changing?
Promising Breakthroughs (2024–2025)
New Diagnostic Tools
• MicroRNA panels and blood-based biomarkers are showing promise as non-invasive ways to detect endometriosis earlier.
• Advanced imaging like high-resolution MRI and ultrasound with specialized protocols are helping detect lesions more reliably.
Endometriosis Foundation: Emerging Research: https://www.endofound.org/news-research
PubMed: Biomarkers in Endometriosis: https://pubmed.ncbi.nlm.nih.gov/30807918/
AI & Machine Learning
Artificial intelligence is being trained to analyze symptom patterns, scan images, and even detect potential markers in menstrual blood—offering hope for faster, more accurate screening in the near future.
More Funding and Advocacy
• Governments and nonprofits are increasing research grants.
• Social media and support groups are amplifying women’s voices and experiences.
• Healthcare providers are receiving more training in pelvic pain and minimally invasive surgical options like excision surgery.

What This Means for You (or Someone You Love)
Faster, less invasive diagnosis is on the horizon.
Women are being believed and supported more than ever.
With better understanding comes more targeted treatment options, like hormonal therapies, dietary approaches, pelvic floor therapy, and expert excision surgery.
What You Can Do Right Now
1. Track your symptoms: Keep a daily journal of pain, mood, fatigue, and cycle details.
2. Advocate for yourself: Ask your doctor about excision surgery vs. ablation. A specialist is necessary for proper endometriosis care. Unfortunately, your typical OB-GYN is not an endometriosis or excision specialist.
3. Get support: You're not alone. Online communities and advocacy organizations offer connection and practical help.
Nancy’s Nook Endometriosis Education Group: https://www.facebook.com/groups/NancysNookEndoEd
Center for Endometriosis Care: https://www.centerforendo.com/
Why This Matters
Endometriosis is a whole-body disease that can affect a woman’s physical, emotional, and reproductive health. We are just starting to make some noise & bring attention to this disease and other hormonal diseases related to it.
“The future of women’s health is shifting—but only if we keep raising our voices.”
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.

My Story: Caitlin

I’ve never had “normal” periods. Growing up, I thought it was normal to take ibuprofen around the clock. It wasn’t something we talked about much, so I didn’t know any different.
In high school, I developed gastroparesis, never imagining it could be connected to my periods—especially since my symptoms didn’t look like most patients’. Over the years, I also experienced stabbing pains that were often brushed off as burst cysts.
In my 20s and 30s, I struggled with getting and staying pregnant. Thankfully, I was able to safely deliver two healthy babies, and during that time I had no gastroparesis symptoms at all. But after pregnancy, my periods worsened, and my gastroparesis came roaring back. I sought help from a midwife/nutritionist, multiple OBGYNs, and several dietitians. Despite eating healthy, exercising, and having perfect bloodwork, I kept gaining weight and bloating without explanation. My belly never seemed to match the rest of my body, and for half the month I was completely drained of energy.
In February 2020, I had my first exploratory surgery. The surgeon told me, “There was some growth, but I’d bet money it’s not endo.” The pathology came back positive for endometriosis. I was put into medicinal menopause right as the pandemic shut everything down, and so began a five-year journey: two more excision surgeries, nerve block injections, countless physical therapy sessions. Yet my symptoms kept flaring. I often felt like I was losing my mind—my body was showing clear symptoms, but little could be done to help.
I’m fortunate to have excellent health insurance, because otherwise I could have bought a small second house with what’s been spent on my care. For three years, I was in physical therapy for hip pain and limited mobility—pain my doctor could see during exams, but that never showed up on scans. During my second excision surgery, they found an endo mass, and the pain disappeared afterward (though mobility issues remained).
Working in front of hundreds of people, I constantly worried whether my clothes would still fit by the end of the day due to bloating. I could also tell when I was nearing the need for another excision surgery because I’d break out with painful cystic acne.
Finally, in June 2025, I sought out a new surgeon who specialized in endometriosis. For the first time—other than with my physical therapist—I felt truly heard. She explained the disease in a way that finally made sense. I chose to have a hysterectomy. During surgery, they found one ovary fused to my bladder and endometriosis in multiple places, despite my last excision only eight months earlier. The most shocking part? I had less pain the day after surgery than I did before. Even more surprising, I haven’t had any gastroparesis symptoms since. My surgeon said there’s no research showing a link, but she wasn’t surprised. Sadly, I wasn’t surprised either that research hasn’t been done on these links.
Now, about six weeks post-op, my body is healing, but the emotional scars remain. It’s one thing to choose not to have more children—it’s another to have that choice permanently taken away. I still battle anxiety around food, since my body spent years tying certain meals to painful symptoms. I also fear for my daughter. Anytime she has GI issues, I worry she might inherit this disease.
I’ve been blessed with supportive family and friends, a great workplace, and the financial means to access care. Even with all of that, it still took me 15–20 years from my first symptoms to get a diagnosis.
I share my story in the hope that organizations like Our Daughters Foundation can help change this. By speaking openly about what’s often considered a taboo subject, I want to spare someone else the years of pain I endured.
