Breaking the Silence: Why Endometriosis Took So Long to Be Taken Seriously
—and What’s Finally Changing
For millions of women around the world, the story of endometriosis is one of pain,
dismissal, and delay. But after decades of silence, the tide is beginning to turn.
Breaking the Silence:
Why Endometriosis Took So Long to Be Taken Seriously
—and What’s Finally Changing
For millions of women around the world, the story of endometriosis is one of pain,
dismissal, and delay. But after decades of silence, the tide is beginning to turn.
What Is Endometriosis—and Why Has It Been Ignored for So Long
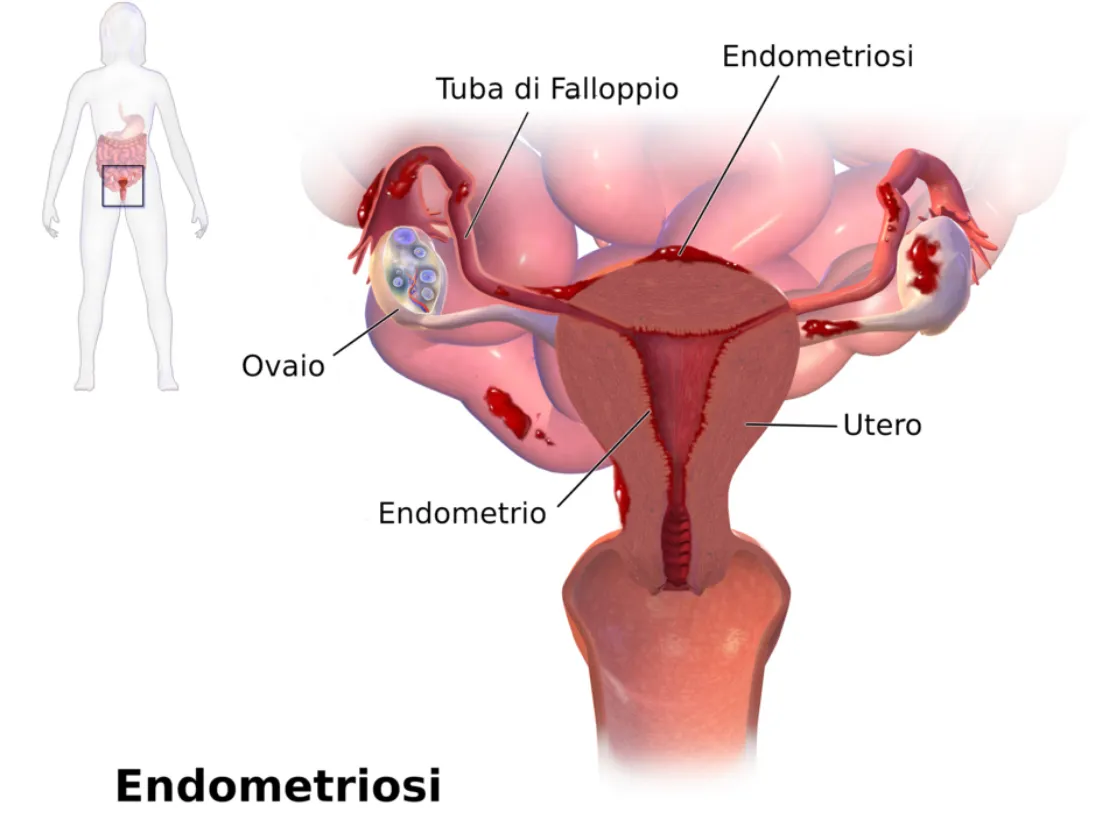
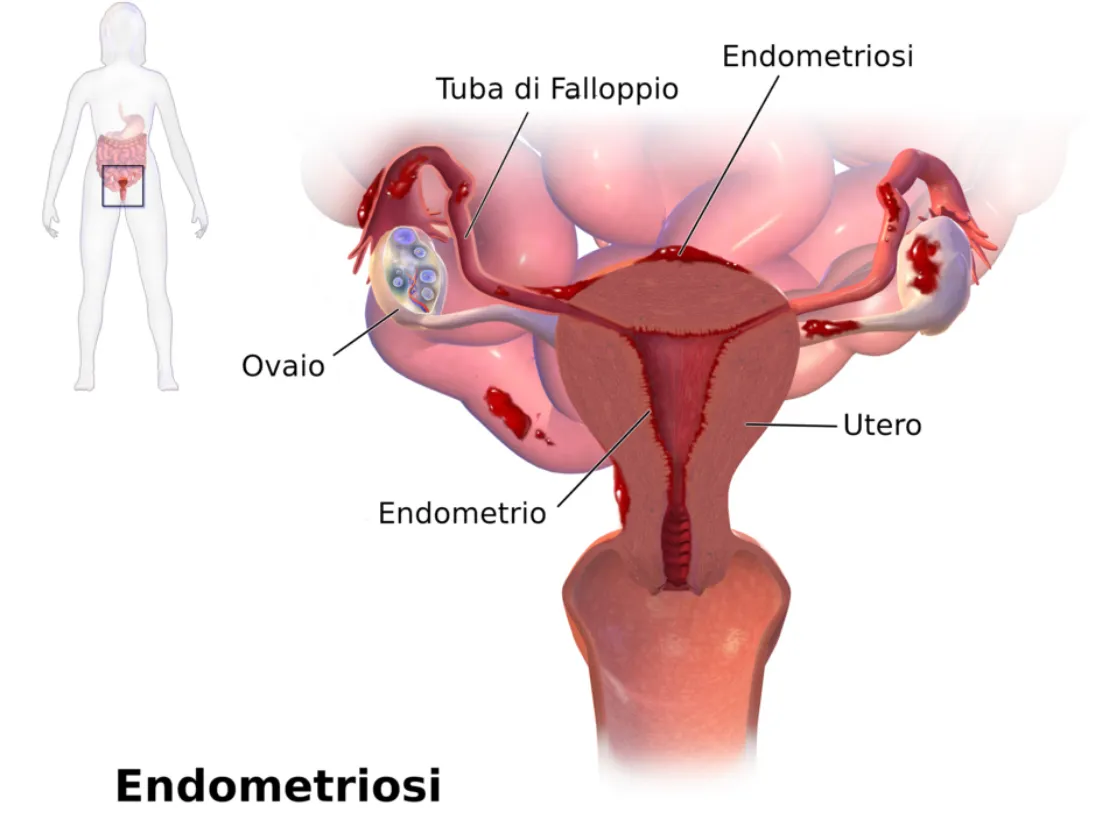
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus grows outside the uterus—on the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond. This tissue responds to hormonal changes, leading to inflammation, scarring, and severe pain.
Despite affecting roughly 1 in 10 women of reproductive age worldwide, endometriosis has historically been misunderstood, underdiagnosed, and mistreated.
World Health Organization Fact Sheet on Endometriosis:
https://www.who.int/news-room/fact-sheets/detail/endometriosis
The Average Time to Diagnosis? Still Over 7 Years.
That’s not a typo. On average, it takes 7 to 10 years from the first symptoms to a correct diagnosis. Why?
• Symptoms are often normalized: Severe period pain? “Just part of being a woman.”
• Lack of non-invasive testing: Diagnosis has long relied on laparoscopic surgery.
• Medical gaps: Many healthcare providers, including OB-GYN’s, receive limited training in gynecologic pain conditions.
NIH: Delays in Endometriosis Diagnosis: https://pubmed.ncbi.nlm.nih.gov/32147966/
What Are the Symptoms of Endometriosis?

Every woman’s experience is different, but some of the most common symptoms include:
• Intense pelvic or abdominal pain
• Pain during or after sex
• Heavy or irregular periods
• Chronic fatigue
• Gastrointestinal issues like bloating, nausea, or constipation
• Infertility or difficulty conceiving
What’s Finally Changing?
Promising Breakthroughs (2024–2025)
New Diagnostic Tools
• MicroRNA panels and blood-based biomarkers are showing promise as non-invasive ways to detect endometriosis earlier.
• Advanced imaging like high-resolution MRI and ultrasound with specialized protocols are helping detect lesions more reliably.
Endometriosis Foundation: Emerging Research: https://www.endofound.org/news-research
PubMed: Biomarkers in Endometriosis: https://pubmed.ncbi.nlm.nih.gov/30807918/
AI & Machine Learning
Artificial intelligence is being trained to analyze symptom patterns, scan images, and even detect potential markers in menstrual blood—offering hope for faster, more accurate screening in the near future.
More Funding and Advocacy
• Governments and nonprofits are increasing research grants.
• Social media and support groups are amplifying women’s voices and experiences.
• Healthcare providers are receiving more training in pelvic pain and minimally invasive surgical options like excision surgery.

What This Means for You (or Someone You Love)
Faster, less invasive diagnosis is on the horizon.
Women are being believed and supported more than ever.
With better understanding comes more targeted treatment options, like hormonal therapies, dietary approaches, pelvic floor therapy, and expert excision surgery.
What You Can Do Right Now
1. Track your symptoms: Keep a daily journal of pain, mood, fatigue, and cycle details.
2. Advocate for yourself: Ask your doctor about excision surgery vs. ablation. A specialist is necessary for proper endometriosis care. Unfortunately, your typical OB-GYN is not an endometriosis or excision specialist.
3. Get support: You're not alone. Online communities and advocacy organizations offer connection and practical help.
Nancy’s Nook Endometriosis Education Group: https://www.facebook.com/groups/NancysNookEndoEd
Center for Endometriosis Care: https://www.centerforendo.com/
Why This Matters
Endometriosis is a whole-body disease that can affect a woman’s physical, emotional, and reproductive health. We are just starting to make some noise & bring attention to this disease and other hormonal diseases related to it.
“The future of women’s health is shifting—but only if we keep raising our voices.”
What Is Endometriosis—and Why Has It Been Ignored for So Long
Endometriosis is a chronic, often painful condition where tissue similar to the lining of the uterus grows outside the uterus—on the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond. This tissue responds to hormonal changes, leading to inflammation, scarring, and severe pain.
Despite affecting roughly 1 in 10 women of reproductive age worldwide, endometriosis has historically been misunderstood, underdiagnosed, and mistreated.
World Health Organization Fact Sheet on Endometriosis:
https://www.who.int/news-room/fact-sheets/detail/endometriosis
The Average Time to Diagnosis? Still Over 7 Years.
That’s not a typo. On average, it takes 7 to 10 years from the first symptoms to a correct diagnosis. Why?
• Symptoms are often normalized: Severe period pain? “Just part of being a woman.”
• Lack of non-invasive testing: Diagnosis has long relied on laparoscopic surgery.
• Medical gaps: Many healthcare providers, including OB-GYN’s, receive limited training in gynecologic pain conditions.
NIH: Delays in Endometriosis Diagnosis: https://pubmed.ncbi.nlm.nih.gov/32147966/
What Are the Symptoms of Endometriosis?

Every woman’s experience is different, but some of the most common symptoms include:
• Intense pelvic or abdominal pain
• Pain during or after sex
• Heavy or irregular periods
• Chronic fatigue
• Gastrointestinal issues like bloating, nausea, or constipation
• Infertility or difficulty conceiving
What’s Finally Changing?
Promising Breakthroughs (2024–2025)
New Diagnostic Tools
• MicroRNA panels and blood-based biomarkers are showing promise as non-invasive ways to detect endometriosis earlier.
• Advanced imaging like high-resolution MRI and ultrasound with specialized protocols are helping detect lesions more reliably.
Endometriosis Foundation: Emerging Research: https://www.endofound.org/news-research
PubMed: Biomarkers in Endometriosis: https://pubmed.ncbi.nlm.nih.gov/30807918/
AI & Machine Learning
Artificial intelligence is being trained to analyze symptom patterns, scan images, and even detect potential markers in menstrual blood—offering hope for faster, more accurate screening in the near future.
More Funding and Advocacy
• Governments and nonprofits are increasing research grants.
• Social media and support groups are amplifying women’s voices and experiences.
• Healthcare providers are receiving more training in pelvic pain and minimally invasive surgical options like excision surgery.

What This Means for You (or Someone You Love)
Faster, less invasive diagnosis is on the horizon.
Women are being believed and supported more than ever.
With better understanding comes more targeted treatment options, like hormonal therapies, dietary approaches, pelvic floor therapy, and expert excision surgery.
What You Can Do Right Now
1. Track your symptoms: Keep a daily journal of pain, mood, fatigue, and cycle details.
2. Advocate for yourself: Ask your doctor about excision surgery vs. ablation. A specialist is necessary for proper endometriosis care. Unfortunately, your typical OB-GYN is not an endometriosis or excision specialist.
3. Get support: You're not alone. Online communities and advocacy organizations offer connection and practical help.
Nancy’s Nook Endometriosis Education Group: https://www.facebook.com/groups/NancysNookEndoEd
Center for Endometriosis Care: https://www.centerforendo.com/
Why This Matters
Endometriosis is a whole-body disease that can affect a woman’s physical, emotional, and reproductive health. We are just starting to make some noise & bring attention to this disease and other hormonal diseases related to it.
“The future of women’s health is shifting—but only if we keep raising our voices.”
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.

My Story: Allison

"I honestly can’t remember a time when my monthly cycles felt “normal.” From early on, they were always painful—something I learned to dread every single month. I had symptoms that I now know aren’t normal, but back then, I just assumed this was how it was supposed to be.
My symptoms affected both my physical and mental health. The abdominal pain and cramping would leave me doubled over, sometimes unable to move. I experienced nausea, vomiting, dizziness, and terrible headaches. But even more difficult were the days when anxiety took over so completely that the simple act of getting out of bed would trigger a panic attack. All I could do was lay there, waiting for the wave to pass, hoping I could eventually function at even the most basic level.
Over time, this pattern began to erode my daily life. I was told over and over again that I just had “bad cycles,” and that hormonal birth control was the only option. I tried it and quickly realized it wasn’t sustainable for me. The other response I often got was silence—or worse: “suck it up,” “push through it,” “this is just part of being a woman.” So I did what I thought I had to do: I learned to silently suffer, white-knuckling my way through each month.
By the time I reached my thirties, after having my two sweet kids, I only had about 5 or 6 days each month where I could carry out everyday tasks without pain or debilitating symptoms. I was barely making it through. That’s when I knew something had to change—I couldn’t keep living like this.
I hadn’t considered endometriosis until my twin sister, who had gone through very similar experiences, was diagnosed after several surgeries. Her story opened the door for me to seek answers of my own. With the support of a trusted doctor, I underwent testing. They suspected both endometriosis and adenomyosis.
A few months later, I had surgery. It confirmed both diagnoses. My uterus was removed due to adenomyosis, and endometriosis was also found and excised. That surgery gave me my life back. And I don’t say that lightly. For the first time in decades, I wasn’t confined to my bed. I didn’t have to plan my life around pain. I could move, breathe, think, and live. My kids had their mom back.
Some symptoms have returned in recent months, but this time I’m not doing it alone. I’m working closely with two practitioners—one addressing things holistically, the other exploring surgical options if needed. I feel supported, seen, and hopeful.
What I’ve learned through all of this is that far too many women are suffering in silence—dismissed, minimized, and left without answers. We’re told that this is just the way it is. But it doesn’t have to be.
That’s why I’m so incredibly grateful for Our Daughters Foundation and for people like Kara, who are bringing attention, support, and real solutions to parts of women’s health that have been ignored for far too long. Being told to “tough it out” leaves one feeling isolated. Knowing something’s wrong but not being sure if anyone will help you—that’s a different kind of pain.
Awareness changes that. Advocacy changes that. Community changes that.
Thank you, Our Daughters Foundation, for fighting for us—for helping women everywhere feel less alone, and for making it known that “just a bad period” is never something we should accept."
-Allie
