Are Endometriosis, Adenomyosis, and PCOS Autoimmune Conditions?
By Our Daughters Foundation
More and more women are asking an important question: Could my hormone-related illness also be connected to my immune system?
Conditions like endometriosis, adenomyosis, and polycystic ovary syndrome (PCOS) are often discussed in the context of reproductive health or hormonal imbalance. But researchers are beginning to explore deeper connections—specifically, whether autoimmunity plays a role in these diseases.
Let’s break down what the science says—and what questions remain unanswered.
Are Endometriosis, Adenomyosis, and PCOS Autoimmune Conditions?
By Our Daughters Foundation
More and more women are asking an important question: Could my hormone-related illness also be connected to my immune system?
Conditions like endometriosis, adenomyosis, and polycystic ovary syndrome (PCOS) are often discussed in the context of reproductive health or hormonal imbalance. But researchers are beginning to explore deeper connections—specifically, whether autoimmunity plays a role in these diseases.
Let’s break down what the science says—and what questions remain unanswered.
What Is Autoimmunity?
The immune system is designed to protect the body from threats like viruses and bacteria. But in autoimmune diseases, the immune system becomes misguided and starts attacking the body’s own cells and tissues.
Common autoimmune conditions include:
• Lupus
• Rheumatoid arthritis
• Hashimoto’s thyroiditis
• Multiple sclerosis
Symptoms vary widely, but many autoimmune conditions involve chronic inflammation, pain, fatigue, and a pattern of flare-ups.

The Immune System and Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus—causing pain, inflammation, and sometimes infertility. While its exact cause is still debated, many researchers believe that the immune system fails to clear out these rogue cells effectively.
Several studies have found:
• Women with endometriosis often have higher levels of inflammatory markers, like cytokines and prostaglandins.
• Natural killer (NK) cell activity is lower in women with endometriosis, impairing the immune system’s ability to destroy misplaced cells.
• There are elevated autoantibodies in some patients, suggesting an autoimmune component.
Some scientists now consider endometriosis to be a non-classical autoimmune disease—showing many features of one without meeting all diagnostic criteria.
Further reading:
• NIH - Immune dysfunction in endometriosis: https://pubmed.ncbi.nlm.nih.gov/30664929/
• Cleveland Clinic - Endometriosis and the Immune System: https://health.clevelandclinic.org/endometriosis-and-the-immune-system/
What About Adenomyosis?
Adenomyosis is sometimes called the "sister disease" of endometriosis. It occurs when endometrial tissue grows into the muscular wall of the uterus. It's less studied, but immune abnormalities have also been observed.
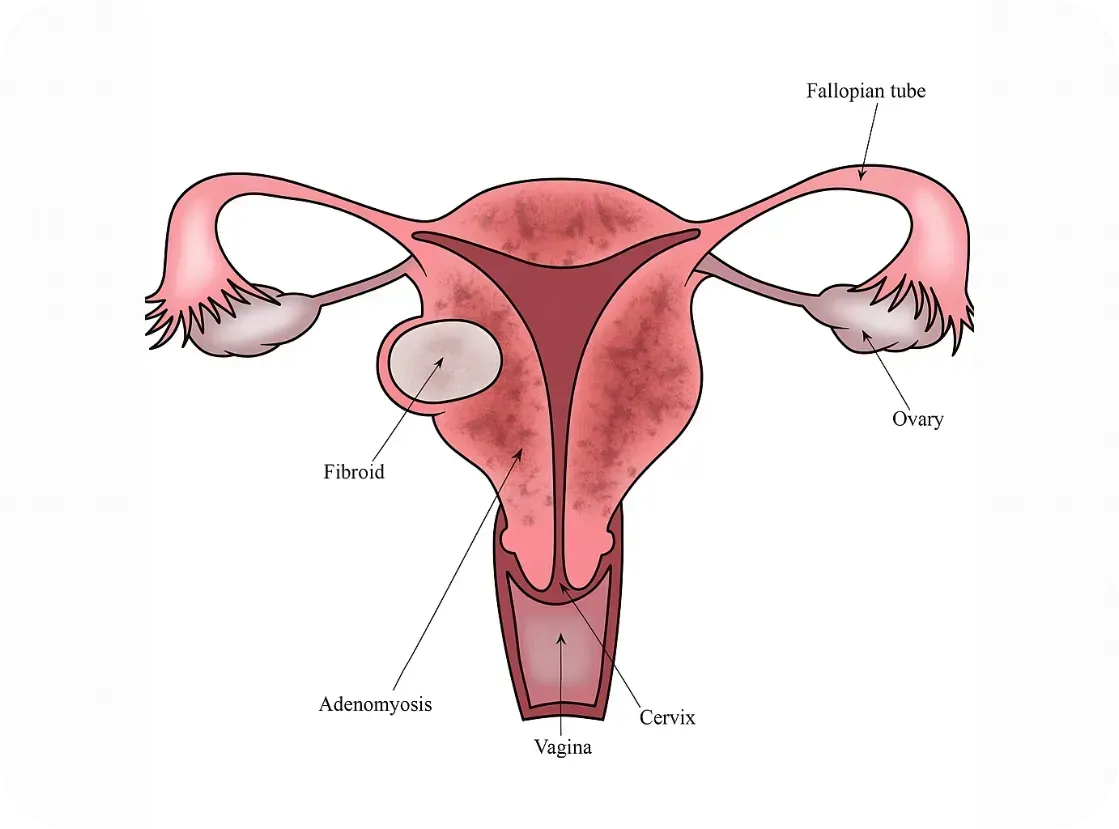
Research is still emerging, but here’s what we know:
• Women with adenomyosis show immune cell changes and chronic inflammation within the uterus.
• Some studies report increased macrophage and mast cell activity—cells involved in both immune defense and inflammation
• The condition often coexists with endometriosis, raising questions about shared immune pathways.
While it’s too early to label adenomyosis an autoimmune disorder, it may involve an immune imbalance that contributes to symptoms.
Further reading:
• Frontiers in Immunology - Immunopathogenesis of Adenomyosis: https://www.frontiersin.org/articles/10.3389/fimmu.2021.796273/full
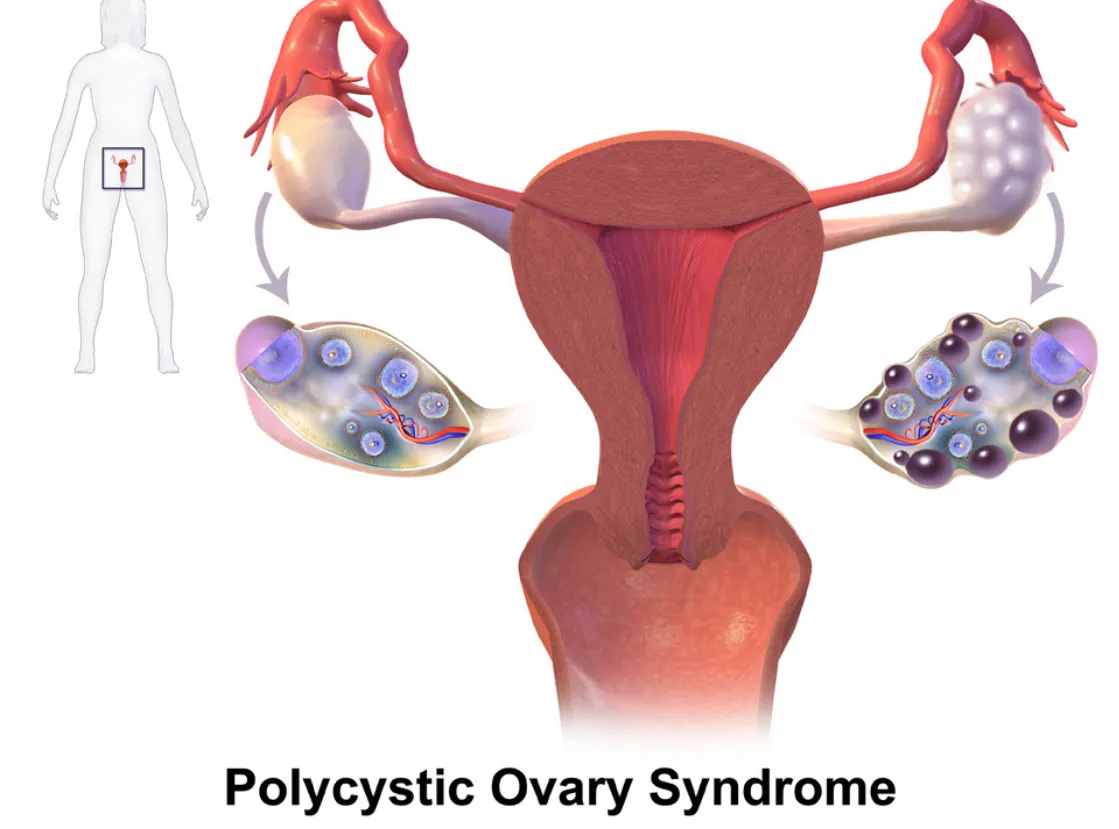
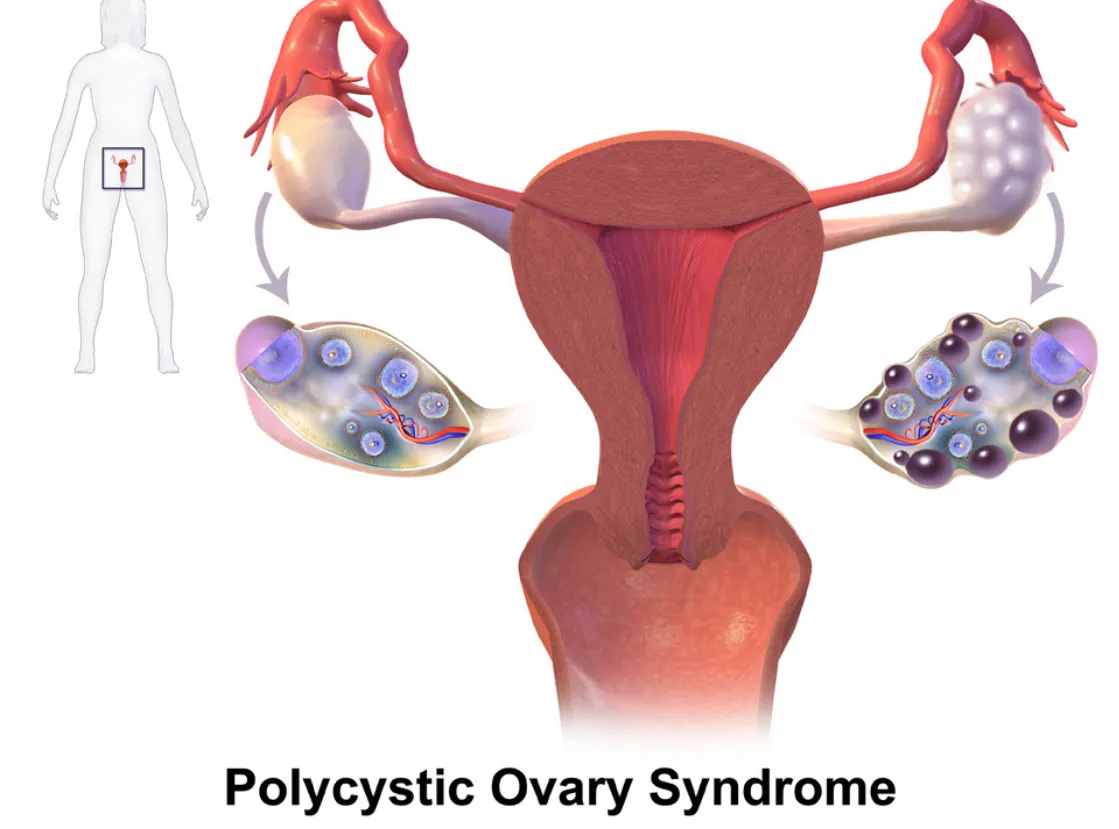
PCOS and Autoimmune Overlap
Polycystic ovary syndrome (PCOS) is primarily known as a hormonal disorder involving androgen excess and insulin resistance. However, there’s growing interest in its immune connections, especially in women with chronic inflammation or thyroid issues.
Emerging links include:
• Hashimoto’s thyroiditis (an autoimmune thyroid disorder) is more common in women with PCOS.
• Inflammatory markers like C-reactive protein (CRP) are often elevated in PCOS patients.
• Some PCOS patients have anti-ovarian antibodies, suggesting potential autoimmunity.
Still, the autoimmune theory is more speculative in PCOS than in endometriosis.
Further reading:
Further reading:
• Journal of Clinical Endocrinology & Metabolism - PCOS and Autoimmune Disease: https://academic.oup.com/jcem/article/106/9/e3536/6280755
Why Does This Matter?
If immune dysfunction is part of the puzzle, treatment strategies may need to shift. Many women with endometriosis, adenomyosis, or PCOS are treated solely with hormone suppression—but if autoimmunity is involved, we may also need to address inflammation, gut health, and immune regulation.
There’s also hope that newer treatments—like immunomodulatory therapies or even personalized nutrition and lifestyle interventions—could improve outcomes when tailored to the immune system’s role.
Bottom Line
We don’t yet have all the answers, but the research is evolving. Endometriosis, adenomyosis, and PCOS may not be traditional autoimmune diseases—but they often coexist with immune dysfunction, and the overlap deserves attention. At Our Daughters Foundation, we believe in honoring women’s voices, advocating for deeper research, and pursuing whole-body solutions.
If you’ve experienced overlapping conditions like endo, thyroid disease, or unexplained inflammation—you’re not alone.
What Is Autoimmunity?
The immune system is designed to protect the body from threats like viruses and bacteria. But in autoimmune diseases, the immune system becomes misguided and starts attacking the body’s own cells and tissues.
Common autoimmune conditions include:
• Lupus
• Rheumatoid arthritis
• Hashimoto’s thyroiditis
• Multiple sclerosis
Symptoms vary widely, but many autoimmune conditions involve chronic inflammation, pain, fatigue, and a pattern of flare-ups.

The Immune System and Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus—causing pain, inflammation, and sometimes infertility. While its exact cause is still debated, many researchers believe that the immune system fails to clear out these rogue cells effectively.
Several studies have found:
• Women with endometriosis often have higher levels of inflammatory markers, like cytokines and prostaglandins.
• Natural killer (NK) cell activity is lower in women with endometriosis, impairing the immune system’s ability to destroy misplaced cells.
• There are elevated autoantibodies in some patients, suggesting an autoimmune component.
Some scientists now consider endometriosis to be a non-classical autoimmune disease—showing many features of one without meeting all diagnostic criteria.
Further reading:
• NIH - Immune dysfunction in endometriosis: https://pubmed.ncbi.nlm.nih.gov/30664929/
• Cleveland Clinic - Endometriosis and the Immune System: https://health.clevelandclinic.org/endometriosis-and-the-immune-system/
What About Adenomyosis?
Adenomyosis is sometimes called the "sister disease" of endometriosis. It occurs when endometrial tissue grows into the muscular wall of the uterus. It's less studied, but immune abnormalities have also been observed.
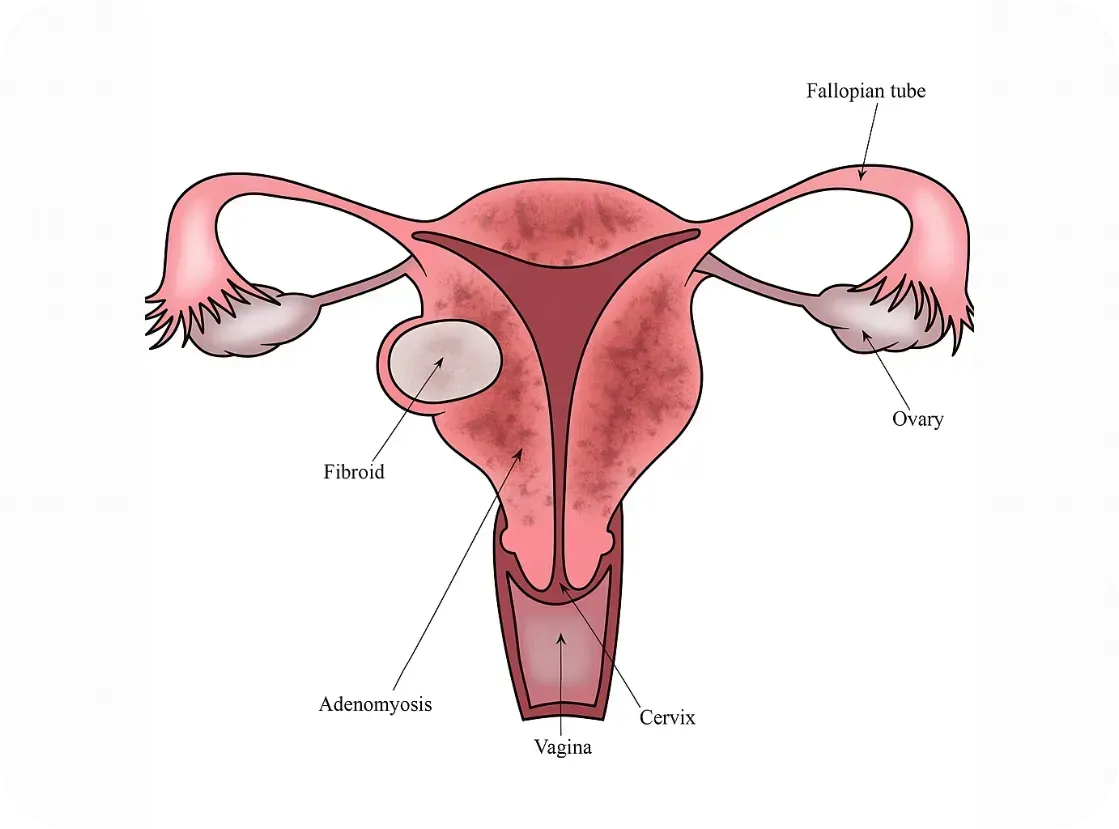
Research is still emerging, but here’s what we know:
• Women with adenomyosis show immune cell changes and chronic inflammation within the uterus.
• Some studies report increased macrophage and mast cell activity—cells involved in both immune defense and inflammation
• The condition often coexists with endometriosis, raising questions about shared immune pathways.
While it’s too early to label adenomyosis an autoimmune disorder, it may involve an immune imbalance that contributes to symptoms.
Further reading:
• Frontiers in Immunology - Immunopathogenesis of Adenomyosis: https://www.frontiersin.org/articles/10.3389/fimmu.2021.796273/full
PCOS and Autoimmune Overlap
Polycystic ovary syndrome (PCOS) is primarily known as a hormonal disorder involving androgen excess and insulin resistance. However, there’s growing interest in its immune connections, especially in women with chronic inflammation or thyroid issues.
Emerging links include:
• Hashimoto’s thyroiditis (an autoimmune thyroid disorder) is more common in women with PCOS.
• Inflammatory markers like C-reactive protein (CRP) are often elevated in PCOS patients.
• Some PCOS patients have anti-ovarian antibodies, suggesting potential autoimmunity.
Still, the autoimmune theory is more speculative in PCOS than in endometriosis.
Further reading:
Further reading:
• Journal of Clinical Endocrinology & Metabolism - PCOS and Autoimmune Disease: https://academic.oup.com/jcem/article/106/9/e3536/6280755
Why Does This Matter?
If immune dysfunction is part of the puzzle, treatment strategies may need to shift. Many women with endometriosis, adenomyosis, or PCOS are treated solely with hormone suppression—but if autoimmunity is involved, we may also need to address inflammation, gut health, and immune regulation.
There’s also hope that newer treatments—like immunomodulatory therapies or even personalized nutrition and lifestyle interventions—could improve outcomes when tailored to the immune system’s role.
Bottom Line
We don’t yet have all the answers, but the research is evolving. Endometriosis, adenomyosis, and PCOS may not be traditional autoimmune diseases—but they often coexist with immune dysfunction, and the overlap deserves attention. At Our Daughters Foundation, we believe in honoring women’s voices, advocating for deeper research, and pursuing whole-body solutions.
If you’ve experienced overlapping conditions like endo, thyroid disease, or unexplained inflammation—you’re not alone.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.

My Story: Kathleen Allen

Hi, I’m Kathleen 👋🏻
I’m a mom to three littles and someone who’s walked a long road with women’s health issues—including endometriosis, adenomyosis, ovarian tumors, and a hysterectomy at just 30 years old.
Ever since my first period, I’ve dealt with difficult cycles — heavy bleeding, intense pain, and vomiting that I thought was just “normal.”
After each of my kids, the pain got worse. By my second pregnancy, I was having regular prodromal labor from 20 weeks on, and during my third, it became so severe I ended up having my son prematurely.
After that, the pain stopped following a monthly pattern and started showing up almost every day. I held onto hope for a fourth child, but eventually found out my uterus was in such poor condition from adenomyosis that it was unlikely I could even carry another pregnancy. It was then that I made the difficult decision to have a hysterectomy.
Not long after my hysterectomy, I was referred to an oncologist and was diagnosed with ovarian tumors along with ongoing endometriosis and hormone-related issues. I’ve also dealt with complications from surgery, like perimenopause, adhesions and scar tissue — things many women quietly live with, often without answers. I am currently under the care of the oncology team and expecting to have another surgery in the near future.
These experiences have shaped the path I’m on now. I went back to school to become a functional nutritionist, driven by a deep belief in healing from the inside out. Food and exercise has played a huge role in helping me reclaim my health. I’m committed to living well and helping other women feel empowered in their own health journeys.
I’m sharing this to help bring more awareness to women’s health — because these stories are more common than we think, and they deserve to be talked about.
