Are Endometriosis, Adenomyosis, and PCOS Autoimmune Conditions?
By Our Daughters Foundation
More and more women are asking an important question: Could my hormone-related illness also be connected to my immune system?
Conditions like endometriosis, adenomyosis, and polycystic ovary syndrome (PCOS) are often discussed in the context of reproductive health or hormonal imbalance. But researchers are beginning to explore deeper connections—specifically, whether autoimmunity plays a role in these diseases.
Let’s break down what the science says—and what questions remain unanswered.
Are Endometriosis, Adenomyosis, and PCOS Autoimmune Conditions?
By Our Daughters Foundation
More and more women are asking an important question: Could my hormone-related illness also be connected to my immune system?
Conditions like endometriosis, adenomyosis, and polycystic ovary syndrome (PCOS) are often discussed in the context of reproductive health or hormonal imbalance. But researchers are beginning to explore deeper connections—specifically, whether autoimmunity plays a role in these diseases.
Let’s break down what the science says—and what questions remain unanswered.
What Is Autoimmunity?
The immune system is designed to protect the body from threats like viruses and bacteria. But in autoimmune diseases, the immune system becomes misguided and starts attacking the body’s own cells and tissues.
Common autoimmune conditions include:
• Lupus
• Rheumatoid arthritis
• Hashimoto’s thyroiditis
• Multiple sclerosis
Symptoms vary widely, but many autoimmune conditions involve chronic inflammation, pain, fatigue, and a pattern of flare-ups.

The Immune System and Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus—causing pain, inflammation, and sometimes infertility. While its exact cause is still debated, many researchers believe that the immune system fails to clear out these rogue cells effectively.
Several studies have found:
• Women with endometriosis often have higher levels of inflammatory markers, like cytokines and prostaglandins.
• Natural killer (NK) cell activity is lower in women with endometriosis, impairing the immune system’s ability to destroy misplaced cells.
• There are elevated autoantibodies in some patients, suggesting an autoimmune component.
Some scientists now consider endometriosis to be a non-classical autoimmune disease—showing many features of one without meeting all diagnostic criteria.
Further reading:
• NIH - Immune dysfunction in endometriosis: https://pubmed.ncbi.nlm.nih.gov/30664929/
• Cleveland Clinic - Endometriosis and the Immune System: https://health.clevelandclinic.org/endometriosis-and-the-immune-system/
What About Adenomyosis?
Adenomyosis is sometimes called the "sister disease" of endometriosis. It occurs when endometrial tissue grows into the muscular wall of the uterus. It's less studied, but immune abnormalities have also been observed.
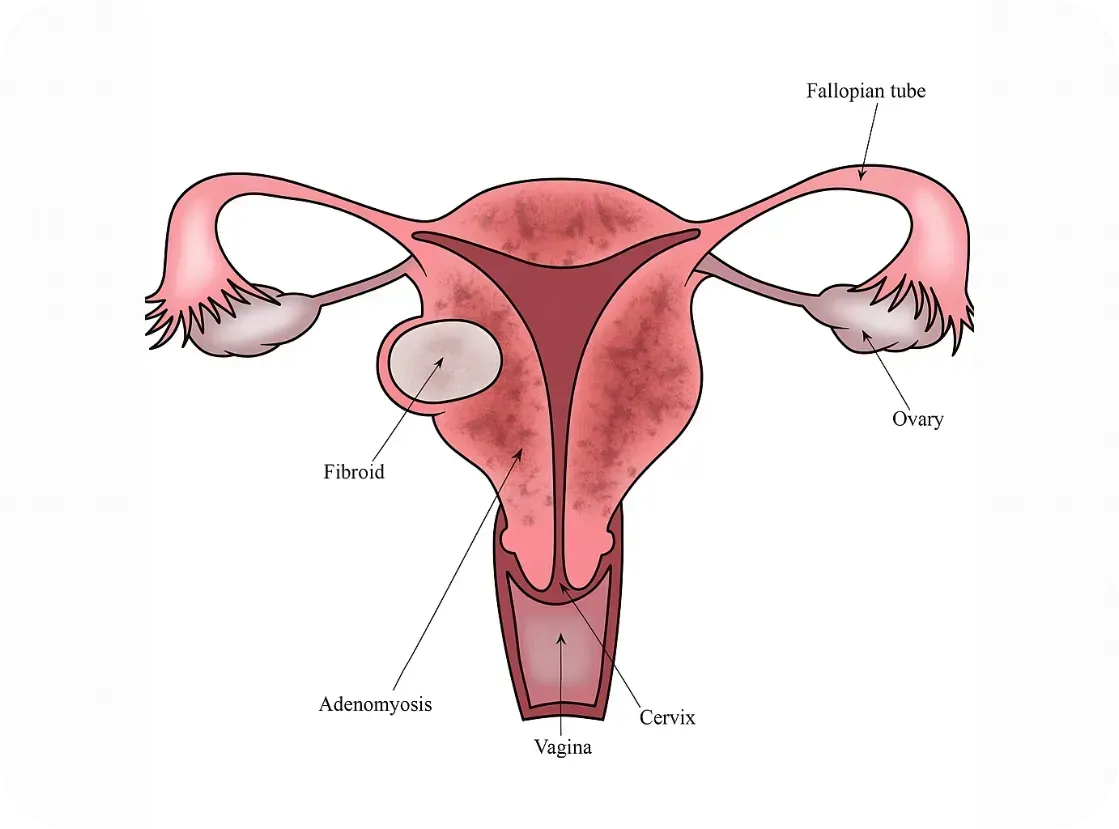
Research is still emerging, but here’s what we know:
• Women with adenomyosis show immune cell changes and chronic inflammation within the uterus.
• Some studies report increased macrophage and mast cell activity—cells involved in both immune defense and inflammation
• The condition often coexists with endometriosis, raising questions about shared immune pathways.
While it’s too early to label adenomyosis an autoimmune disorder, it may involve an immune imbalance that contributes to symptoms.
Further reading:
• Frontiers in Immunology - Immunopathogenesis of Adenomyosis: https://www.frontiersin.org/articles/10.3389/fimmu.2021.796273/full
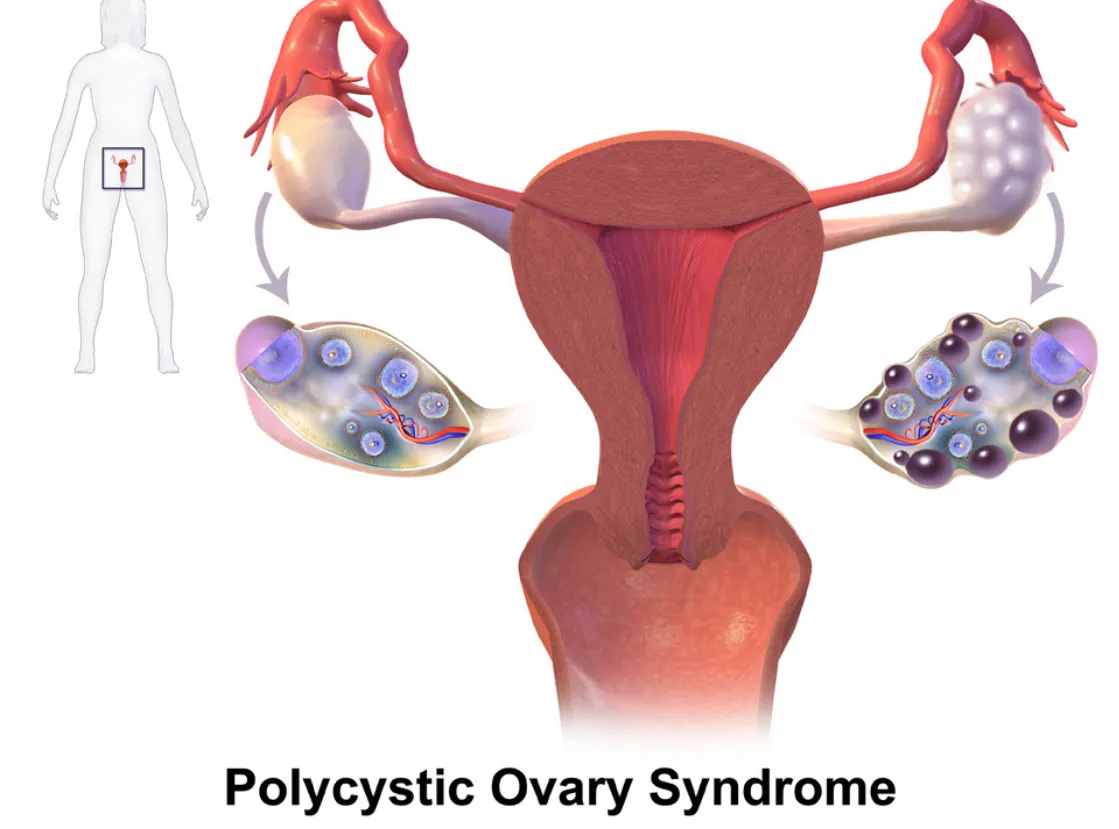
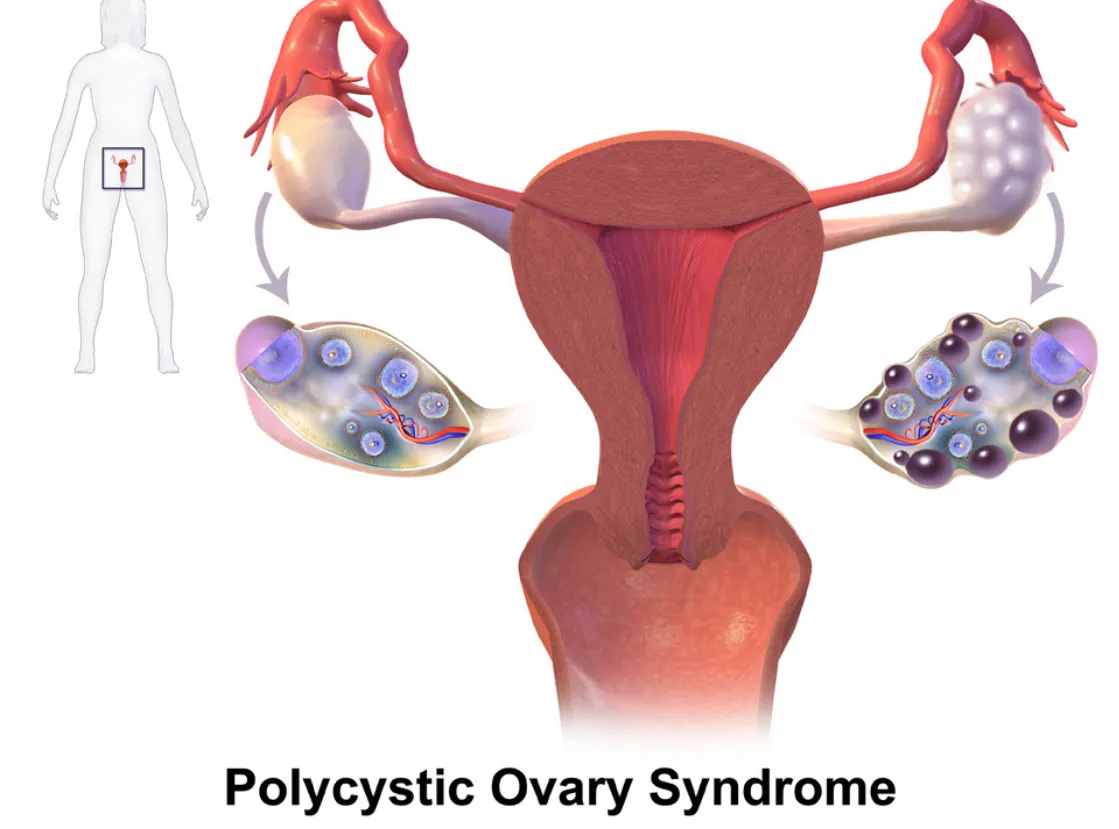
PCOS and Autoimmune Overlap
Polycystic ovary syndrome (PCOS) is primarily known as a hormonal disorder involving androgen excess and insulin resistance. However, there’s growing interest in its immune connections, especially in women with chronic inflammation or thyroid issues.
Emerging links include:
• Hashimoto’s thyroiditis (an autoimmune thyroid disorder) is more common in women with PCOS.
• Inflammatory markers like C-reactive protein (CRP) are often elevated in PCOS patients.
• Some PCOS patients have anti-ovarian antibodies, suggesting potential autoimmunity.
Still, the autoimmune theory is more speculative in PCOS than in endometriosis.
Further reading:
Further reading:
• Journal of Clinical Endocrinology & Metabolism - PCOS and Autoimmune Disease: https://academic.oup.com/jcem/article/106/9/e3536/6280755
Why Does This Matter?
If immune dysfunction is part of the puzzle, treatment strategies may need to shift. Many women with endometriosis, adenomyosis, or PCOS are treated solely with hormone suppression—but if autoimmunity is involved, we may also need to address inflammation, gut health, and immune regulation.
There’s also hope that newer treatments—like immunomodulatory therapies or even personalized nutrition and lifestyle interventions—could improve outcomes when tailored to the immune system’s role.
Bottom Line
We don’t yet have all the answers, but the research is evolving. Endometriosis, adenomyosis, and PCOS may not be traditional autoimmune diseases—but they often coexist with immune dysfunction, and the overlap deserves attention. At Our Daughters Foundation, we believe in honoring women’s voices, advocating for deeper research, and pursuing whole-body solutions.
If you’ve experienced overlapping conditions like endo, thyroid disease, or unexplained inflammation—you’re not alone.
What Is Autoimmunity?
The immune system is designed to protect the body from threats like viruses and bacteria. But in autoimmune diseases, the immune system becomes misguided and starts attacking the body’s own cells and tissues.
Common autoimmune conditions include:
• Lupus
• Rheumatoid arthritis
• Hashimoto’s thyroiditis
• Multiple sclerosis
Symptoms vary widely, but many autoimmune conditions involve chronic inflammation, pain, fatigue, and a pattern of flare-ups.

The Immune System and Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus—causing pain, inflammation, and sometimes infertility. While its exact cause is still debated, many researchers believe that the immune system fails to clear out these rogue cells effectively.
Several studies have found:
• Women with endometriosis often have higher levels of inflammatory markers, like cytokines and prostaglandins.
• Natural killer (NK) cell activity is lower in women with endometriosis, impairing the immune system’s ability to destroy misplaced cells.
• There are elevated autoantibodies in some patients, suggesting an autoimmune component.
Some scientists now consider endometriosis to be a non-classical autoimmune disease—showing many features of one without meeting all diagnostic criteria.
Further reading:
• NIH - Immune dysfunction in endometriosis: https://pubmed.ncbi.nlm.nih.gov/30664929/
• Cleveland Clinic - Endometriosis and the Immune System: https://health.clevelandclinic.org/endometriosis-and-the-immune-system/
What About Adenomyosis?
Adenomyosis is sometimes called the "sister disease" of endometriosis. It occurs when endometrial tissue grows into the muscular wall of the uterus. It's less studied, but immune abnormalities have also been observed.
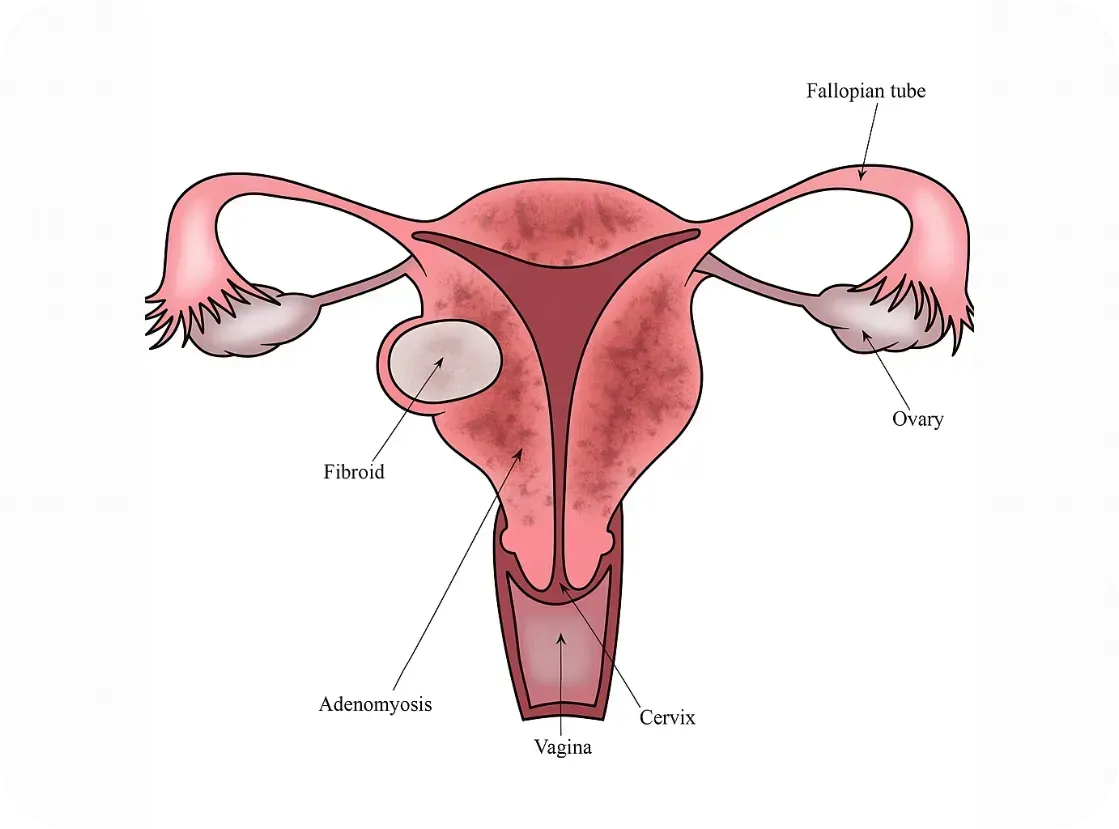
Research is still emerging, but here’s what we know:
• Women with adenomyosis show immune cell changes and chronic inflammation within the uterus.
• Some studies report increased macrophage and mast cell activity—cells involved in both immune defense and inflammation
• The condition often coexists with endometriosis, raising questions about shared immune pathways.
While it’s too early to label adenomyosis an autoimmune disorder, it may involve an immune imbalance that contributes to symptoms.
Further reading:
• Frontiers in Immunology - Immunopathogenesis of Adenomyosis: https://www.frontiersin.org/articles/10.3389/fimmu.2021.796273/full
PCOS and Autoimmune Overlap
Polycystic ovary syndrome (PCOS) is primarily known as a hormonal disorder involving androgen excess and insulin resistance. However, there’s growing interest in its immune connections, especially in women with chronic inflammation or thyroid issues.
Emerging links include:
• Hashimoto’s thyroiditis (an autoimmune thyroid disorder) is more common in women with PCOS.
• Inflammatory markers like C-reactive protein (CRP) are often elevated in PCOS patients.
• Some PCOS patients have anti-ovarian antibodies, suggesting potential autoimmunity.
Still, the autoimmune theory is more speculative in PCOS than in endometriosis.
Further reading:
Further reading:
• Journal of Clinical Endocrinology & Metabolism - PCOS and Autoimmune Disease: https://academic.oup.com/jcem/article/106/9/e3536/6280755
Why Does This Matter?
If immune dysfunction is part of the puzzle, treatment strategies may need to shift. Many women with endometriosis, adenomyosis, or PCOS are treated solely with hormone suppression—but if autoimmunity is involved, we may also need to address inflammation, gut health, and immune regulation.
There’s also hope that newer treatments—like immunomodulatory therapies or even personalized nutrition and lifestyle interventions—could improve outcomes when tailored to the immune system’s role.
Bottom Line
We don’t yet have all the answers, but the research is evolving. Endometriosis, adenomyosis, and PCOS may not be traditional autoimmune diseases—but they often coexist with immune dysfunction, and the overlap deserves attention. At Our Daughters Foundation, we believe in honoring women’s voices, advocating for deeper research, and pursuing whole-body solutions.
If you’ve experienced overlapping conditions like endo, thyroid disease, or unexplained inflammation—you’re not alone.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
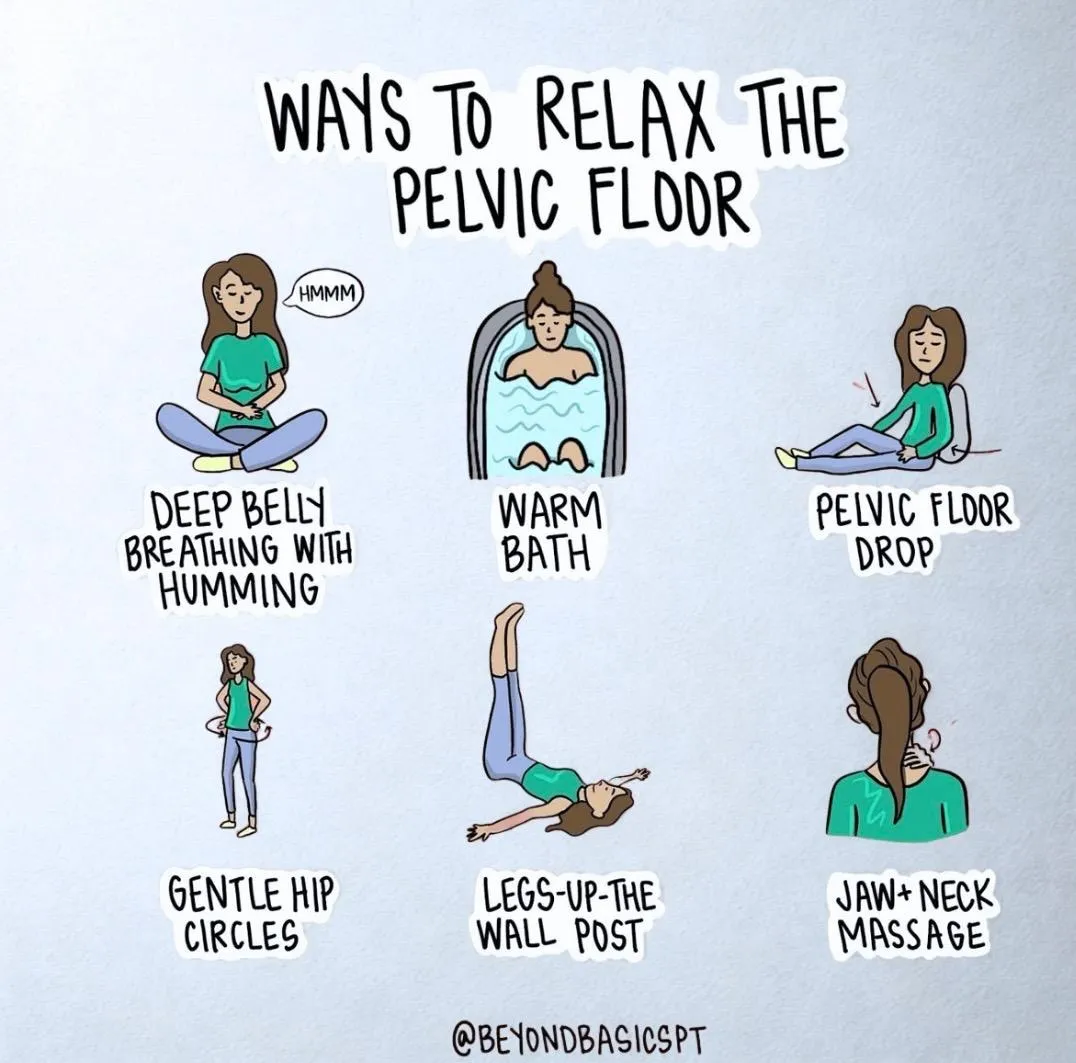
Relaxing Your Pelvic Floor
Relaxing the Pelvic Floor: Simple Practices with Powerful Benefits
Tension in the pelvic floor is more common than many realize—and it can be a significant source of pain, dysfunction, and stress. While most people have heard of Kegels to strengthen pelvic floor muscles, the equally important skill of relaxing those muscles is often overlooked. Chronic tightness in the pelvic floor can lead to a range of symptoms including pelvic pain, urinary urgency, painful intercourse, constipation, and low back pain.
*Your pelvic floor carries a lot—physically and emotionally. Incorporating simple tools like these into your daily routine isn’t just about relief after symptoms hit—it’s about building a system that might help prevent them before they start. A few minutes of deep breathing, gentle movement, or a warm bath can help calm your nervous system, ease tension, and support your body.That said, flare-ups aren’t always in your control—and that doesn’t mean you’re doing anything wrong. This is the nature of endometriosis. These are just supportive tools, not a cure—but sometimes, little things can make a big difference.
Fortunately, simple daily techniques—like the ones illustrated by @beyondbasicspt in the graphic above—can make a profound difference. Let’s break down each method and explore what the research says.
1. Deep Belly Breathing with Humming
Slow diaphragmatic breathing encourages the pelvic floor to relax naturally. When you inhale deeply, your diaphragm moves downward, and this movement is mirrored by the pelvic floor, creating a gentle stretch and release.
Why add humming? Humming stimulates the vagus nerve, which activates the parasympathetic nervous system (the “rest and digest” response), helping the entire pelvic region soften.
Research Insight: A 2020 study published in Pain Medicine found that slow, diaphragmatic breathing improved outcomes in patients with chronic pelvic pain by reducing muscle tone and improving nervous system regulation (Mehling et al., 2020).
2. Warm Bath
Immersion in warm water increases blood flow and reduces muscle guarding—especially in the pelvic area. The buoyancy also helps reduce gravitational compression, encouraging muscle relaxation.
Research Insight: Hydrotherapy has long been shown to reduce muscle tension and improve circulation (Kamioka et al., 2010). For pelvic pain specifically, warmth and hydrostatic pressure may help ease myofascial tension in the pelvic floor.
3. Pelvic Floor Drop (Let-Go Technique)
Unlike Kegels (which focus on contraction), the pelvic floor drop emphasizes releasing and lengthening the pelvic muscles. Think of it as the "exhale and let go" moment for the pelvic floor.
Research Insight: A 2016 review in the Journal of Bodywork and Movement Therapies emphasizes that relaxation techniques—including conscious "letting go"—are key in treating non-relaxing pelvic floor dysfunction (FitzGerald et al., 2016).
4. Gentle Hip Circles
These rhythmic movements help mobilize the hips and pelvis, gently loosening fascia and improving circulation in the pelvic region.
Research Insight: Movement therapies that increase pelvic mobility are beneficial in reducing hypertonicity (muscle overactivity) in the pelvic floor (Haugstad et al., 2006).
5. Legs-Up-The-Wall Pose
Known as Viparita Karani in yoga, this pose promotes venous return and encourages full-body relaxation. It also reduces pressure in the pelvic region and helps calm the nervous system.
Research Insight: A 2013 study in Evidence-Based Complementary and Alternative Medicine noted that restorative yoga poses, like legs-up-the-wall, reduce sympathetic nervous system activity and improve muscle tone regulation (Telles et al., 2013).
6. Jaw + Neck Massage
Here’s a fascinating link: the jaw and the pelvic floor are neurologically and developmentally connected. Tension in one area often reflects or reinforces tension in the other.
Tip: Try gently massaging the base of your skull and jawline—or even releasing your tongue from the roof of your mouth—to help the pelvic muscles relax.
Research Insight: Somatic connections between the jaw and pelvis have been observed in body-oriented therapies. A 2021 review published in Medical Hypotheses proposed shared motor control pathways that link craniofacial and pelvic floor muscle groups (Wallden, 2021).
Final Thoughts
Pelvic floor relaxation isn’t just about relieving pain—it’s about restoring balance, function, and a sense of ease in the body. Whether you’re dealing with pelvic pain, recovering from childbirth, or simply seeking more mind-body awareness, these gentle practices are worth integrating into your daily routine.
As always, if you're experiencing persistent pelvic discomfort, consult a pelvic floor physical therapist for a personalized plan. These professionals can guide you through both strengthening and relaxation techniques safely.
References
Mehling, W. E., et al. (2020). Effects of breathing retraining on chronic pelvic pain. Pain Medicine, 21(4), 798–808.
Kamioka, H., et al. (2010). Effectiveness of aquatic exercise and balneotherapy: A summary of systematic reviews. Journal of Epidemiology, 20(1), 2–12.
FitzGerald, M. P., et al. (2016). Evaluation and treatment of non-relaxing pelvic floor dysfunction. J Bodyw Mov Ther, 20(2), 275–281.
Haugstad, G. K., et al. (2006). Muscular and non-muscular responses to movement therapy in women with chronic pelvic pain. Physiotherapy Research International, 11(4), 217–228.
Telles, S., et al. (2013). Restorative yoga for women with pelvic pain: a randomized controlled trial. Evid Based Complement Alternat Med, 2013, 792581.
Wallden, M. (2021). The anatomical and neurobiological link between the jaw and pelvic floor. Medical Hypotheses, 150, 110556.
