Are Endometriosis, Adenomyosis, and PCOS Autoimmune Conditions?
By Our Daughters Foundation
More and more women are asking an important question: Could my hormone-related illness also be connected to my immune system?
Conditions like endometriosis, adenomyosis, and polycystic ovary syndrome (PCOS) are often discussed in the context of reproductive health or hormonal imbalance. But researchers are beginning to explore deeper connections—specifically, whether autoimmunity plays a role in these diseases.
Let’s break down what the science says—and what questions remain unanswered.
Are Endometriosis, Adenomyosis, and PCOS Autoimmune Conditions?
By Our Daughters Foundation
More and more women are asking an important question: Could my hormone-related illness also be connected to my immune system?
Conditions like endometriosis, adenomyosis, and polycystic ovary syndrome (PCOS) are often discussed in the context of reproductive health or hormonal imbalance. But researchers are beginning to explore deeper connections—specifically, whether autoimmunity plays a role in these diseases.
Let’s break down what the science says—and what questions remain unanswered.
What Is Autoimmunity?
The immune system is designed to protect the body from threats like viruses and bacteria. But in autoimmune diseases, the immune system becomes misguided and starts attacking the body’s own cells and tissues.
Common autoimmune conditions include:
• Lupus
• Rheumatoid arthritis
• Hashimoto’s thyroiditis
• Multiple sclerosis
Symptoms vary widely, but many autoimmune conditions involve chronic inflammation, pain, fatigue, and a pattern of flare-ups.

The Immune System and Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus—causing pain, inflammation, and sometimes infertility. While its exact cause is still debated, many researchers believe that the immune system fails to clear out these rogue cells effectively.
Several studies have found:
• Women with endometriosis often have higher levels of inflammatory markers, like cytokines and prostaglandins.
• Natural killer (NK) cell activity is lower in women with endometriosis, impairing the immune system’s ability to destroy misplaced cells.
• There are elevated autoantibodies in some patients, suggesting an autoimmune component.
Some scientists now consider endometriosis to be a non-classical autoimmune disease—showing many features of one without meeting all diagnostic criteria.
Further reading:
• NIH - Immune dysfunction in endometriosis: https://pubmed.ncbi.nlm.nih.gov/30664929/
• Cleveland Clinic - Endometriosis and the Immune System: https://health.clevelandclinic.org/endometriosis-and-the-immune-system/
What About Adenomyosis?
Adenomyosis is sometimes called the "sister disease" of endometriosis. It occurs when endometrial tissue grows into the muscular wall of the uterus. It's less studied, but immune abnormalities have also been observed.
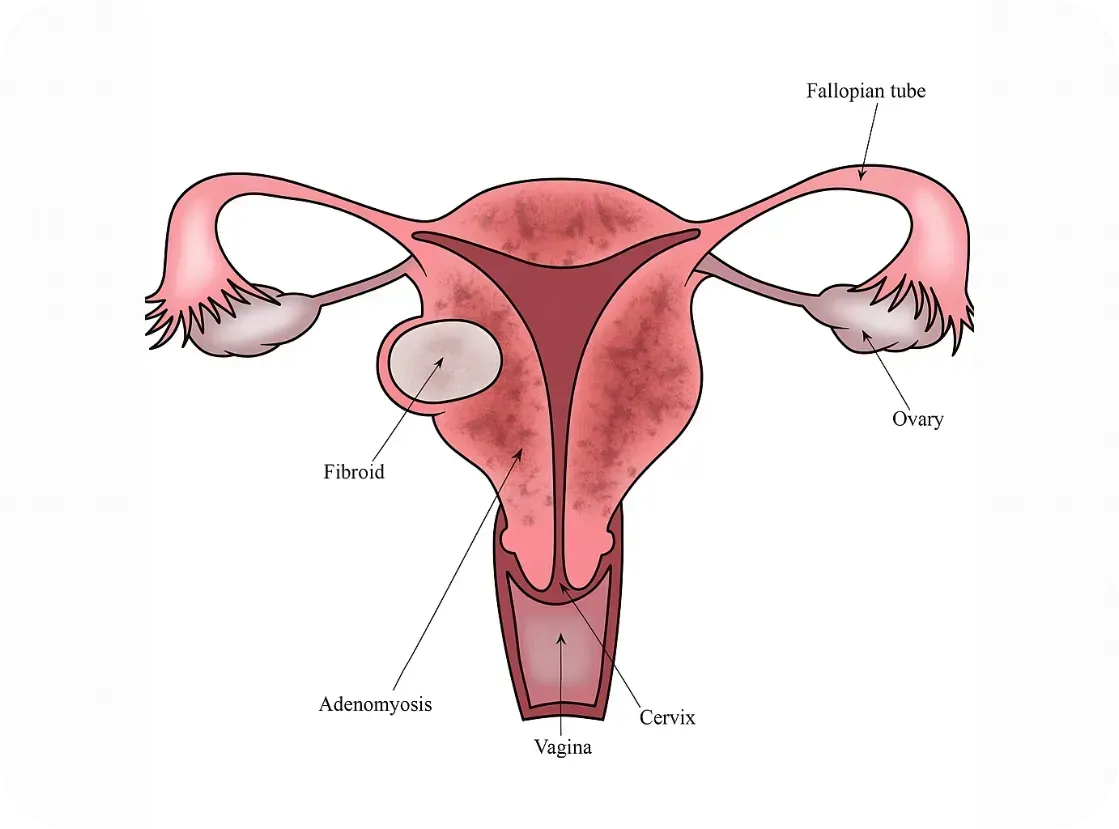
Research is still emerging, but here’s what we know:
• Women with adenomyosis show immune cell changes and chronic inflammation within the uterus.
• Some studies report increased macrophage and mast cell activity—cells involved in both immune defense and inflammation
• The condition often coexists with endometriosis, raising questions about shared immune pathways.
While it’s too early to label adenomyosis an autoimmune disorder, it may involve an immune imbalance that contributes to symptoms.
Further reading:
• Frontiers in Immunology - Immunopathogenesis of Adenomyosis: https://www.frontiersin.org/articles/10.3389/fimmu.2021.796273/full
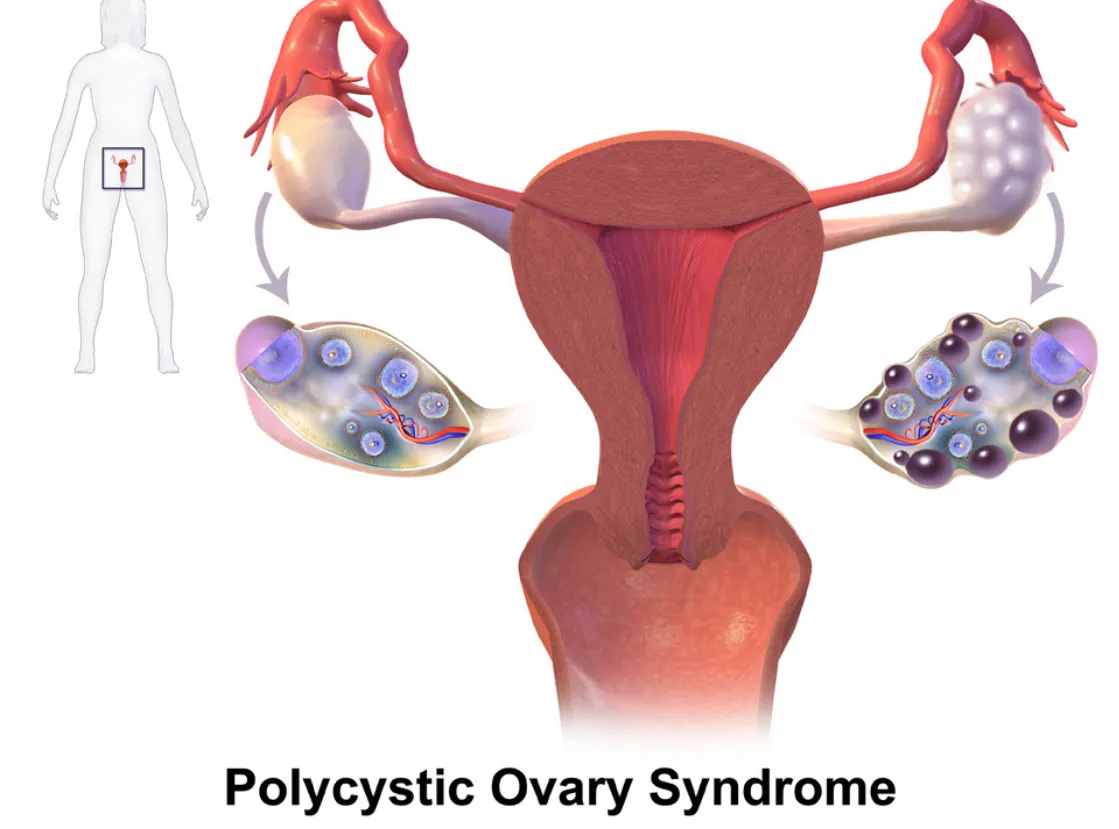
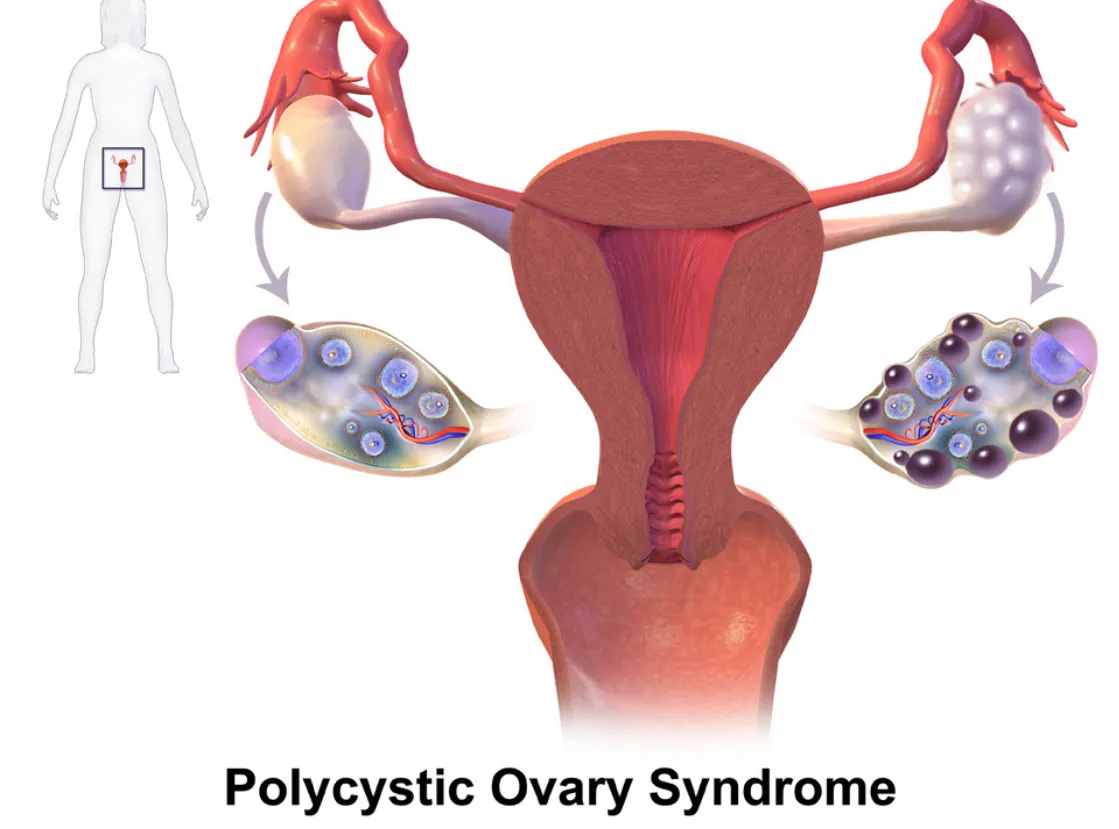
PCOS and Autoimmune Overlap
Polycystic ovary syndrome (PCOS) is primarily known as a hormonal disorder involving androgen excess and insulin resistance. However, there’s growing interest in its immune connections, especially in women with chronic inflammation or thyroid issues.
Emerging links include:
• Hashimoto’s thyroiditis (an autoimmune thyroid disorder) is more common in women with PCOS.
• Inflammatory markers like C-reactive protein (CRP) are often elevated in PCOS patients.
• Some PCOS patients have anti-ovarian antibodies, suggesting potential autoimmunity.
Still, the autoimmune theory is more speculative in PCOS than in endometriosis.
Further reading:
Further reading:
• Journal of Clinical Endocrinology & Metabolism - PCOS and Autoimmune Disease: https://academic.oup.com/jcem/article/106/9/e3536/6280755
Why Does This Matter?
If immune dysfunction is part of the puzzle, treatment strategies may need to shift. Many women with endometriosis, adenomyosis, or PCOS are treated solely with hormone suppression—but if autoimmunity is involved, we may also need to address inflammation, gut health, and immune regulation.
There’s also hope that newer treatments—like immunomodulatory therapies or even personalized nutrition and lifestyle interventions—could improve outcomes when tailored to the immune system’s role.
Bottom Line
We don’t yet have all the answers, but the research is evolving. Endometriosis, adenomyosis, and PCOS may not be traditional autoimmune diseases—but they often coexist with immune dysfunction, and the overlap deserves attention. At Our Daughters Foundation, we believe in honoring women’s voices, advocating for deeper research, and pursuing whole-body solutions.
If you’ve experienced overlapping conditions like endo, thyroid disease, or unexplained inflammation—you’re not alone.
What Is Autoimmunity?
The immune system is designed to protect the body from threats like viruses and bacteria. But in autoimmune diseases, the immune system becomes misguided and starts attacking the body’s own cells and tissues.
Common autoimmune conditions include:
• Lupus
• Rheumatoid arthritis
• Hashimoto’s thyroiditis
• Multiple sclerosis
Symptoms vary widely, but many autoimmune conditions involve chronic inflammation, pain, fatigue, and a pattern of flare-ups.

The Immune System and Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus—causing pain, inflammation, and sometimes infertility. While its exact cause is still debated, many researchers believe that the immune system fails to clear out these rogue cells effectively.
Several studies have found:
• Women with endometriosis often have higher levels of inflammatory markers, like cytokines and prostaglandins.
• Natural killer (NK) cell activity is lower in women with endometriosis, impairing the immune system’s ability to destroy misplaced cells.
• There are elevated autoantibodies in some patients, suggesting an autoimmune component.
Some scientists now consider endometriosis to be a non-classical autoimmune disease—showing many features of one without meeting all diagnostic criteria.
Further reading:
• NIH - Immune dysfunction in endometriosis: https://pubmed.ncbi.nlm.nih.gov/30664929/
• Cleveland Clinic - Endometriosis and the Immune System: https://health.clevelandclinic.org/endometriosis-and-the-immune-system/
What About Adenomyosis?
Adenomyosis is sometimes called the "sister disease" of endometriosis. It occurs when endometrial tissue grows into the muscular wall of the uterus. It's less studied, but immune abnormalities have also been observed.
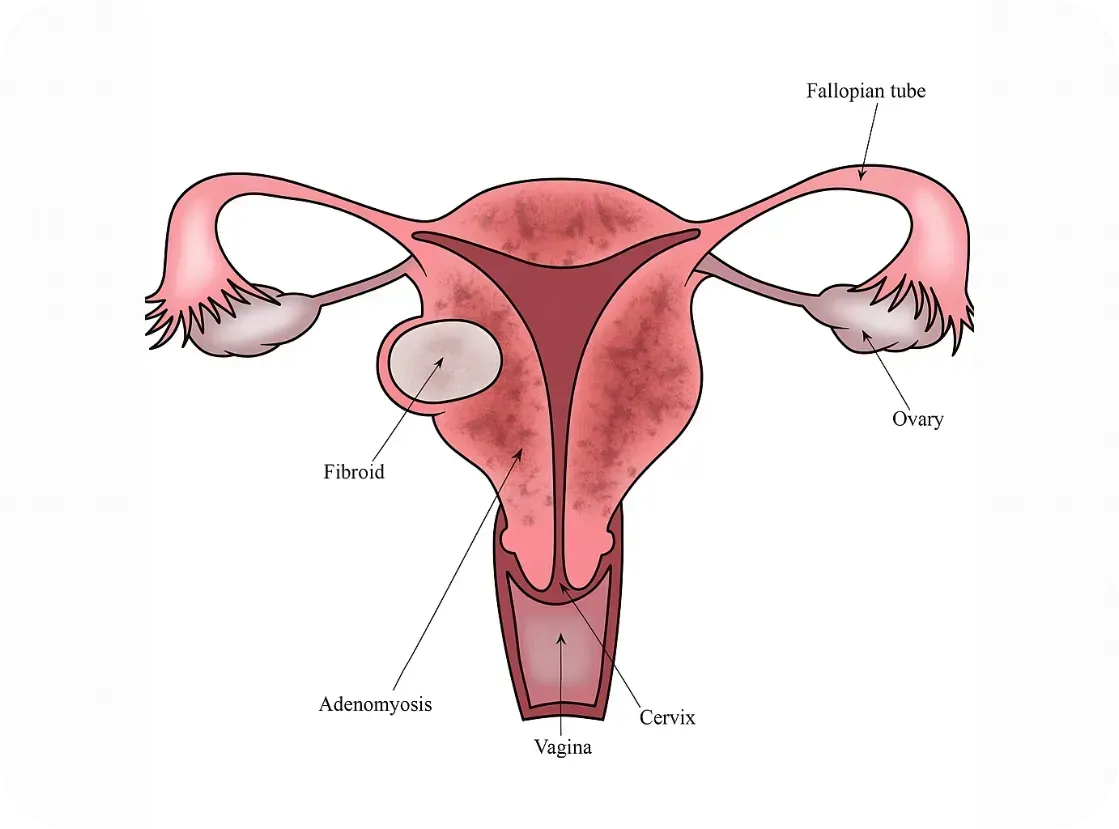
Research is still emerging, but here’s what we know:
• Women with adenomyosis show immune cell changes and chronic inflammation within the uterus.
• Some studies report increased macrophage and mast cell activity—cells involved in both immune defense and inflammation
• The condition often coexists with endometriosis, raising questions about shared immune pathways.
While it’s too early to label adenomyosis an autoimmune disorder, it may involve an immune imbalance that contributes to symptoms.
Further reading:
• Frontiers in Immunology - Immunopathogenesis of Adenomyosis: https://www.frontiersin.org/articles/10.3389/fimmu.2021.796273/full
PCOS and Autoimmune Overlap
Polycystic ovary syndrome (PCOS) is primarily known as a hormonal disorder involving androgen excess and insulin resistance. However, there’s growing interest in its immune connections, especially in women with chronic inflammation or thyroid issues.
Emerging links include:
• Hashimoto’s thyroiditis (an autoimmune thyroid disorder) is more common in women with PCOS.
• Inflammatory markers like C-reactive protein (CRP) are often elevated in PCOS patients.
• Some PCOS patients have anti-ovarian antibodies, suggesting potential autoimmunity.
Still, the autoimmune theory is more speculative in PCOS than in endometriosis.
Further reading:
Further reading:
• Journal of Clinical Endocrinology & Metabolism - PCOS and Autoimmune Disease: https://academic.oup.com/jcem/article/106/9/e3536/6280755
Why Does This Matter?
If immune dysfunction is part of the puzzle, treatment strategies may need to shift. Many women with endometriosis, adenomyosis, or PCOS are treated solely with hormone suppression—but if autoimmunity is involved, we may also need to address inflammation, gut health, and immune regulation.
There’s also hope that newer treatments—like immunomodulatory therapies or even personalized nutrition and lifestyle interventions—could improve outcomes when tailored to the immune system’s role.
Bottom Line
We don’t yet have all the answers, but the research is evolving. Endometriosis, adenomyosis, and PCOS may not be traditional autoimmune diseases—but they often coexist with immune dysfunction, and the overlap deserves attention. At Our Daughters Foundation, we believe in honoring women’s voices, advocating for deeper research, and pursuing whole-body solutions.
If you’ve experienced overlapping conditions like endo, thyroid disease, or unexplained inflammation—you’re not alone.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
New Breakthroughs For Endometriosis

Hope on the Horizon: Breakthroughs in Endometriosis Research
Living with endometriosis or PCOS or fibroids (or any of the other hormone related, immune system diseases) can feel isolating, frustrating, and hopeless, especially for women who are actively fighting symptoms. We have previously highlighted the delay, dismissal and pain that is part of the experience for many of these women. BUT we also want to bring hope by saying that the landscape is starting to shift. Across the globe, researchers are unlocking new discoveries, philanthropists are investing boldly in women’s health, and for the first time in decades, there’s momentum toward real change. We hope this fills you with HOPE today and helps you to know that you are seen and cared for!
Here’s a look at some of the most hopeful developments reshaping the future of endometriosis care — and why we’re optimistic. (AND why we are doing our own research to know the best and most impactful places to invest our dollars!)
New Science Lighting the Way
Moving beyond hormones and surgery
Most current endometriosis treatments rely on hormonal suppression or invasive surgery — options that often come with serious side effects and don’t prevent recurrence or offer a cure.
But a new wave of research is aiming to change that.
Dichloroacetate (DCA), a metabolic drug once used for mitochondrial disorders, is showing surprising promise. In early clinical trials, it reduced lesion size and eased pain in many participants.
“This is the first time we’ve seen a drug target the energy metabolism of endometriosis cells. It’s a potential game-changer,”
— Professor Andrew Horne, University of Edinburgh
HMI-115, a monoclonal antibody targeting the prolactin receptor, is showing significant reductions in pain in Phase II trials.
“The fact that it’s non-hormonal and well tolerated could transform quality of life for millions,”
— Dr. Thomas D’Hooghe, Global Head of Reproductive Medicine R&D at Merck
More than 20 novel therapies are in development, many focused on immune and inflammatory pathways rather than hormones alone. This could lead to disease-modifying treatments, not just symptom control.
Faster, earlier diagnosis
Delays of 7–10 years from symptom onset to diagnosis are still common. That may soon change.
Big-data work at UCSF has identified patterns in millions of health records that could flag endometriosis earlier.
“We’re using artificial intelligence to see what no single doctor could spot in a lifetime,”
— Dr. Marina Sirota, UCSF Institute for Computational Health Sciences
In Australia, researchers are testing a blood-based biomarker panel that could detect endometriosis non-invasively.
New AI-assisted MRI tools are learning to identify endometriosis lesions with accuracy that rivals expert radiologists.
Dedicated research hubs
In May 2025, the Seckin Endometriosis Research Center opened at Cold Spring Harbor Laboratory, powered by a $10 million gift from the Endometriosis Foundation of America (EndoFound) and matched with another $10 million in institutional funding.
“We are building the infrastructure that has been missing in this field for decades. This is how you accelerate cures,”
— Dr. Bruce Stillman, President, Cold Spring Harbor Laboratory
Philanthropy Is Fueling Breakthroughs
After decades of neglect, private donors are helping rewrite the story of women’s health.
The Bill & Melinda Gates Foundation has pledged $2.5 billion through 2030 toward R&D in women’s health, explicitly including gynecologic conditions like endometriosis.
WHAM (Women’s Health Access Matters) has launched its annual Edge Awards to fund early-career researchers focused on endometriosis, PCOS, and menopause.
The Ainsworth family in Australia donated $50 million to launch the Ainsworth Endometriosis Research Institute at the University of New South Wales — the largest known single gift for endometriosis research to date, with the goal of accelerating the understanding, diagnosis and treatment of endometriosis through “integrated research and global collaboration.”
Melinda Gates donated $100 Million to women’s health in order to accelerate research. She emphasized what so many of us have known and live with the consequences of: women’s diseases have been neglected.
This surge in philanthropy is helping fill the gap where public funding has long fallen short. And the list above is not complete, there are many smaller efforts (like Our Daughters Foundation) that seek to fund research, grants for care, and raise awareness.
“Private investment is finally catching up to the urgency patients have always felt. These dollars are helping researchers pursue the bold, risky ideas that government grants often overlook,”
— Dr. Stacey Missmer, Harvard T.H. Chan School of Public Health
Stories of Hope
Beyond the data and dollars, these breakthroughs are already changing lives.
Ella, diagnosed at 14, was one of the youngest participants in the EPiC DCA trial. After years of missing school and friends, she finally began to get her life back.
“It’s like someone turned the volume down on my pain. I can go to class, see friends, be me again.”
Marisol, who endured five surgeries before finding relief with a newer oral therapy, says:
“For the first time in years, I’m planning my future without fear that pain will ruin it.”
We have also featured stories of hope on our pages to show you that you are not alone in your suffering and we are getting closer to understanding this disease.
🌱 Why We’re Hopeful
Endometriosis research is moving from a trickle to a tide, it’s a slow tide and we have a ways to go, but we are moving in the right direction. More of us are making noise, advocating and giving so that we can make a difference now and for our daughters in the future.
New, non-hormonal therapies are emerging.
Faster, less invasive diagnostics are within reach.
Philanthropy and private investment are pouring unprecedented resources into this space.
And most importantly, patients’ voices are finally driving the agenda.
At Our Daughters Foundation, we believe this momentum is just the beginning. The more we invest in understanding this disease — from immune pathways to diagnostic tools — the faster we can build a future where girls and women no longer lose years to pain. It’s a great time to get involved and actually see positive outcomes!
Join the Momentum
Every gift matters. Every conversation matters.
Together, we can help ensure this moment becomes a movement — and that every daughter has a future free from these often debilitating conditions and diseases.
