The Overlooked Link: Allen-Masters Syndrome and Endometriosis
How a Little-Known Condition Can Complicate Diagnosis and Treatment for Women in Pain
The Overlooked Link: Allen-Masters Syndrome and Endometriosis
How a Little-Known Condition Can Complicate Diagnosis and Treatment for Women in Pain
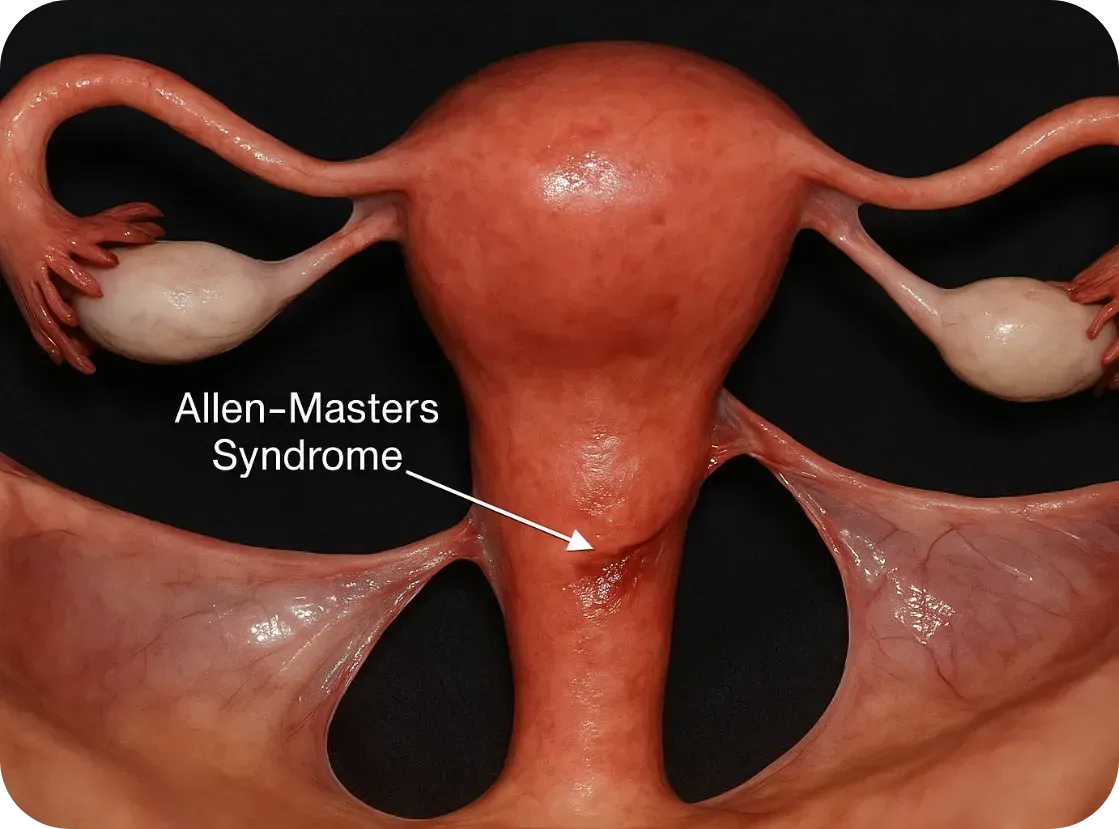
What Is Allen-Masters Syndrome?
Allen-Masters Syndrome (AMS) refers to a condition where the ligaments that support the uterus become torn or stretched, often due to trauma or childbirth. The damage causes the uterus to become hypermobile, or “floppy,” which can lead to chronic pelvic pain, abnormal uterine positioning, and a range of gynecological symptoms.
First described in the 1950s by gynecologists Allen and Masters, the syndrome was initially observed in women who experienced difficult or forceful deliveries. However, it's now known that other pelvic trauma—such as surgeries, repeated inflammation, or even invasive endometriosis—can also play a role.
How It Feels: The Symptoms
The symptoms of AMS often overlap with other pelvic disorders, including endometriosis, which makes it incredibly hard to diagnose:
• Chronic pelvic pain, especially on one side
• Pain during intercourse (dyspareunia)
• A feeling of “heaviness” or dragging in the pelvis
• Irregular bleeding or spotting
• Referred pain to the lower back or legs
• Pain made worse by certain movements or positions
These symptoms can persist even after surgery for endometriosis or fibroids, leaving women frustrated and wondering why their treatments didn’t work.
The Complication with Endometriosis
Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.

Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.
Here’s how:
1. Mimicking or Masking Each Other
AMS pain can feel nearly identical to endometriosis. In laparoscopic surgery, torn ligaments or peritoneal defects might be mistaken for endometriosis—or missed entirely.
2. Worsening Each Other
The uterine instability caused by AMS may increase friction and inflammation in the pelvis, potentially exacerbating endometriosis symptoms. Likewise, the invasive nature of endometriosis can weaken uterine ligaments, creating a cycle of worsening pain.
3. Delaying Diagnosis
Because AMS isn’t well known, many surgeons focus only on excising visible endometriosis lesions. If ligament tears or pelvic instability aren’t also addressed, pain may persist despite "successful" surgery.
4. Influencing Fertility
While endometriosis is a known contributor to infertility, AMS can add to the challenge by altering the position of the uterus, interfering with sperm transport, or making embryo implantation more difficult.
Diagnosis: Why It’s Often Missed
AMS is best diagnosed through clinical examination and often requires a high index of suspicion from an experienced gynecologic surgeon. Imaging like MRI or ultrasound may not show ligament damage clearly. In some cases, laparoscopic exploration is the only way to confirm it, by observing a hypermobile uterus or peritoneal defects (like dimples or windows in the pelvic lining).
Unfortunately, many OB/GYNs are not trained to look for Allen-Masters Syndrome, which means it’s often overlooked—especially in patients already diagnosed with endometriosis
What Can Be Done?
If AMS is suspected, the treatment may include:
• Pelvic physical therapy to support surrounding muscles and reduce pain
• Surgical repair or suspension of the damaged ligaments, often during laparoscopy
• Pain management strategies including nerve blocks or hormonal regulation if endometriosis is also present
• Lifestyle modifications to reduce strain on the pelvis (avoiding certain exercises, managing constipation, etc.)

The Takeaway
Allen-Masters Syndrome may not be as well-known as endometriosis, but its impact is very real—especially for women who feel like they've tried everything and still have no answers.
If you’ve had surgery for endometriosis and your pain persists, or if your symptoms don’t quite fit the typical endo profile, it might be worth asking your doctor about Allen-Masters Syndrome.
Women deserve full answers—not partial relief.
Sources & Further Reading
• Howard FM. (2003). Chronic Pelvic Pain. Obstetrics and Gynecology
• Vercellini P et al. (2006). Chronic pelvic pain: pathogenesis and therapy. Best Practice & Research Clinical Obstetrics and Gynaecology
• Tu FF et al. (2017). Beyond Endometriosis: Recognizing and Treating Comorbid Pelvic Pain Disorders. Clinical Obstetrics and Gynecology
What Is Allen-Masters Syndrome?
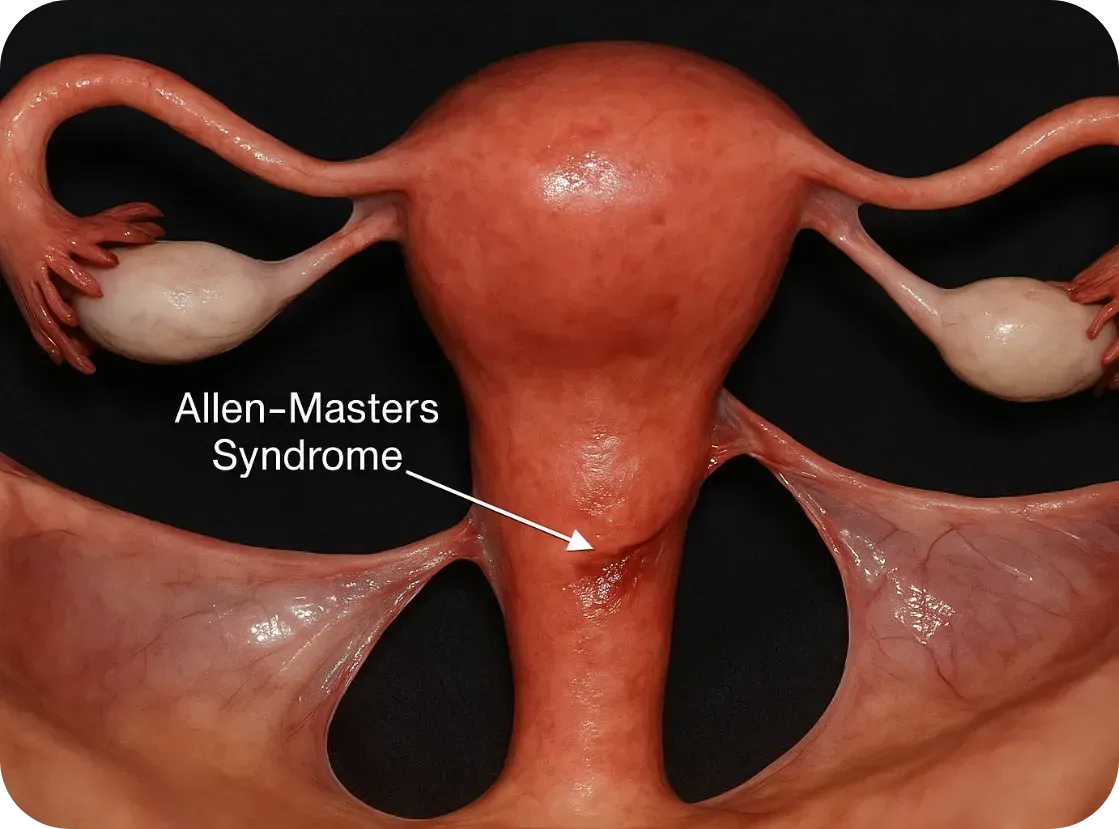
Allen-Masters Syndrome (AMS) refers to a condition where the ligaments that support the uterus become torn or stretched, often due to trauma or childbirth. The damage causes the uterus to become hypermobile, or “floppy,” which can lead to chronic pelvic pain, abnormal uterine positioning, and a range of gynecological symptoms.
First described in the 1950s by gynecologists Allen and Masters, the syndrome was initially observed in women who experienced difficult or forceful deliveries. However, it's now known that other pelvic trauma—such as surgeries, repeated inflammation, or even invasive endometriosis—can also play a role.
How It Feels: The Symptoms
The symptoms of AMS often overlap with other pelvic disorders, including endometriosis, which makes it incredibly hard to diagnose:
• Chronic pelvic pain, especially on one side
• Pain during intercourse (dyspareunia)
• A feeling of “heaviness” or dragging in the pelvis
• Irregular bleeding or spotting
• Referred pain to the lower back or legs
• Pain made worse by certain movements or positions
These symptoms can persist even after surgery for endometriosis or fibroids, leaving women frustrated and wondering why their treatments didn’t work.
The Complication with Endometriosis
Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.

Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.
Here’s how:
1. Mimicking or Masking Each Other
AMS pain can feel nearly identical to endometriosis. In laparoscopic surgery, torn ligaments or peritoneal defects might be mistaken for endometriosis—or missed entirely.
2. Worsening Each Other
The uterine instability caused by AMS may increase friction and inflammation in the pelvis, potentially exacerbating endometriosis symptoms. Likewise, the invasive nature of endometriosis can weaken uterine ligaments, creating a cycle of worsening pain.
3. Delaying Diagnosis
Because AMS isn’t well known, many surgeons focus only on excising visible endometriosis lesions. If ligament tears or pelvic instability aren’t also addressed, pain may persist despite "successful" surgery.
4. Influencing Fertility
While endometriosis is a known contributor to infertility, AMS can add to the challenge by altering the position of the uterus, interfering with sperm transport, or making embryo implantation more difficult.
Diagnosis: Why It’s Often Missed
AMS is best diagnosed through clinical examination and often requires a high index of suspicion from an experienced gynecologic surgeon. Imaging like MRI or ultrasound may not show ligament damage clearly. In some cases, laparoscopic exploration is the only way to confirm it, by observing a hypermobile uterus or peritoneal defects (like dimples or windows in the pelvic lining).
Unfortunately, many OB/GYNs are not trained to look for Allen-Masters Syndrome, which means it’s often overlooked—especially in patients already diagnosed with endometriosis
What Can Be Done?
If AMS is suspected, the treatment may include:
• Pelvic physical therapy to support surrounding muscles and reduce pain
• Surgical repair or suspension of the damaged ligaments, often during laparoscopy
• Pain management strategies including nerve blocks or hormonal regulation if endometriosis is also present
• Lifestyle modifications to reduce strain on the pelvis (avoiding certain exercises, managing constipation, etc.)

The Takeaway
Allen-Masters Syndrome may not be as well-known as endometriosis, but its impact is very real—especially for women who feel like they've tried everything and still have no answers.
If you’ve had surgery for endometriosis and your pain persists, or if your symptoms don’t quite fit the typical endo profile, it might be worth asking your doctor about Allen-Masters Syndrome.
Women deserve full answers—not partial relief.
Sources & Further Reading
• Howard FM. (2003). Chronic Pelvic Pain. Obstetrics and Gynecology
• Vercellini P et al. (2006). Chronic pelvic pain: pathogenesis and therapy. Best Practice & Research Clinical Obstetrics and Gynaecology
• Tu FF et al. (2017). Beyond Endometriosis: Recognizing and Treating Comorbid Pelvic Pain Disorders. Clinical Obstetrics and Gynecology
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.


