The Overlooked Link: Allen-Masters Syndrome and Endometriosis
How a Little-Known Condition Can Complicate Diagnosis and Treatment for Women in Pain
The Overlooked Link: Allen-Masters Syndrome and Endometriosis
How a Little-Known Condition Can Complicate Diagnosis and Treatment for Women in Pain
What Is Allen-Masters Syndrome?
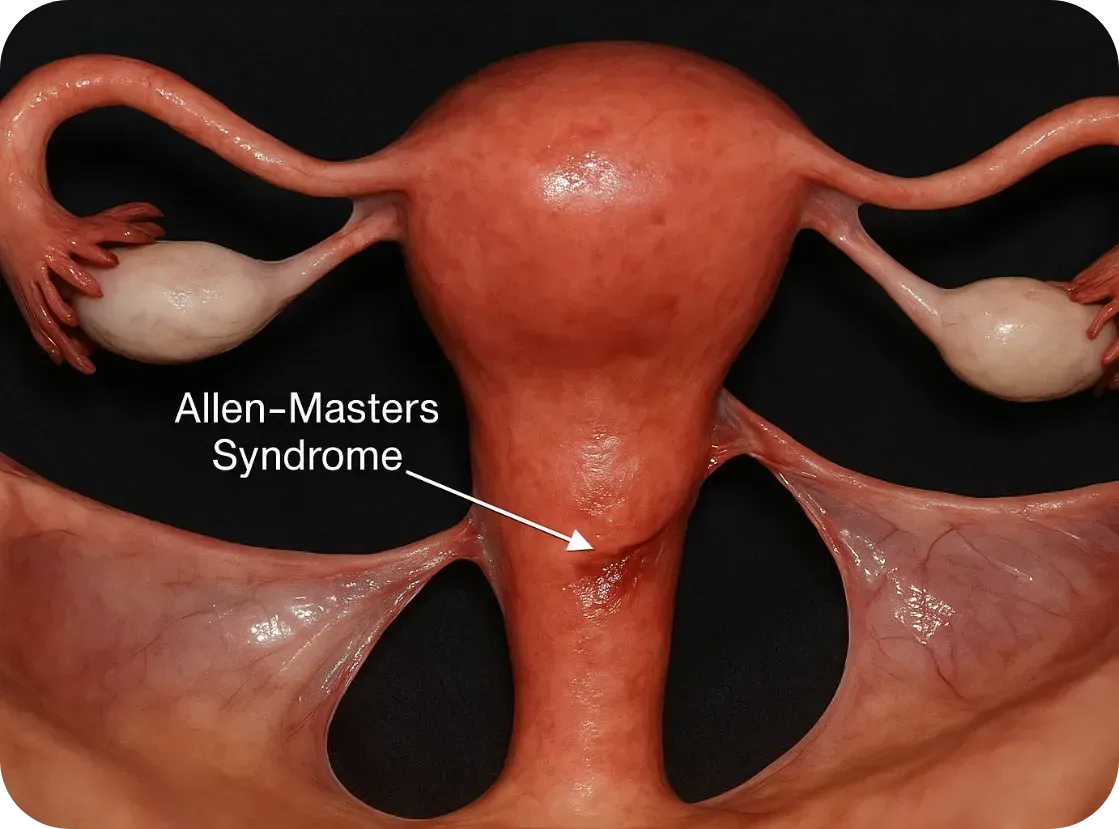
Allen-Masters Syndrome (AMS) refers to a condition where the ligaments that support the uterus become torn or stretched, often due to trauma or childbirth. The damage causes the uterus to become hypermobile, or “floppy,” which can lead to chronic pelvic pain, abnormal uterine positioning, and a range of gynecological symptoms.
First described in the 1950s by gynecologists Allen and Masters, the syndrome was initially observed in women who experienced difficult or forceful deliveries. However, it's now known that other pelvic trauma—such as surgeries, repeated inflammation, or even invasive endometriosis—can also play a role.
How It Feels: The Symptoms
The symptoms of AMS often overlap with other pelvic disorders, including endometriosis, which makes it incredibly hard to diagnose:
• Chronic pelvic pain, especially on one side
• Pain during intercourse (dyspareunia)
• A feeling of “heaviness” or dragging in the pelvis
• Irregular bleeding or spotting
• Referred pain to the lower back or legs
• Pain made worse by certain movements or positions
These symptoms can persist even after surgery for endometriosis or fibroids, leaving women frustrated and wondering why their treatments didn’t work.
The Complication with Endometriosis
Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.

Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.
Here’s how:
1. Mimicking or Masking Each Other
AMS pain can feel nearly identical to endometriosis. In laparoscopic surgery, torn ligaments or peritoneal defects might be mistaken for endometriosis—or missed entirely.
2. Worsening Each Other
The uterine instability caused by AMS may increase friction and inflammation in the pelvis, potentially exacerbating endometriosis symptoms. Likewise, the invasive nature of endometriosis can weaken uterine ligaments, creating a cycle of worsening pain.
3. Delaying Diagnosis
Because AMS isn’t well known, many surgeons focus only on excising visible endometriosis lesions. If ligament tears or pelvic instability aren’t also addressed, pain may persist despite "successful" surgery.
4. Influencing Fertility
While endometriosis is a known contributor to infertility, AMS can add to the challenge by altering the position of the uterus, interfering with sperm transport, or making embryo implantation more difficult.
Diagnosis: Why It’s Often Missed
AMS is best diagnosed through clinical examination and often requires a high index of suspicion from an experienced gynecologic surgeon. Imaging like MRI or ultrasound may not show ligament damage clearly. In some cases, laparoscopic exploration is the only way to confirm it, by observing a hypermobile uterus or peritoneal defects (like dimples or windows in the pelvic lining).
Unfortunately, many OB/GYNs are not trained to look for Allen-Masters Syndrome, which means it’s often overlooked—especially in patients already diagnosed with endometriosis
What Can Be Done?
If AMS is suspected, the treatment may include:
• Pelvic physical therapy to support surrounding muscles and reduce pain
• Surgical repair or suspension of the damaged ligaments, often during laparoscopy
• Pain management strategies including nerve blocks or hormonal regulation if endometriosis is also present
• Lifestyle modifications to reduce strain on the pelvis (avoiding certain exercises, managing constipation, etc.)

The Takeaway
Allen-Masters Syndrome may not be as well-known as endometriosis, but its impact is very real—especially for women who feel like they've tried everything and still have no answers.
If you’ve had surgery for endometriosis and your pain persists, or if your symptoms don’t quite fit the typical endo profile, it might be worth asking your doctor about Allen-Masters Syndrome.
Women deserve full answers—not partial relief.
Sources & Further Reading
• Howard FM. (2003). Chronic Pelvic Pain. Obstetrics and Gynecology
• Vercellini P et al. (2006). Chronic pelvic pain: pathogenesis and therapy. Best Practice & Research Clinical Obstetrics and Gynaecology
• Tu FF et al. (2017). Beyond Endometriosis: Recognizing and Treating Comorbid Pelvic Pain Disorders. Clinical Obstetrics and Gynecology
What Is Allen-Masters Syndrome?
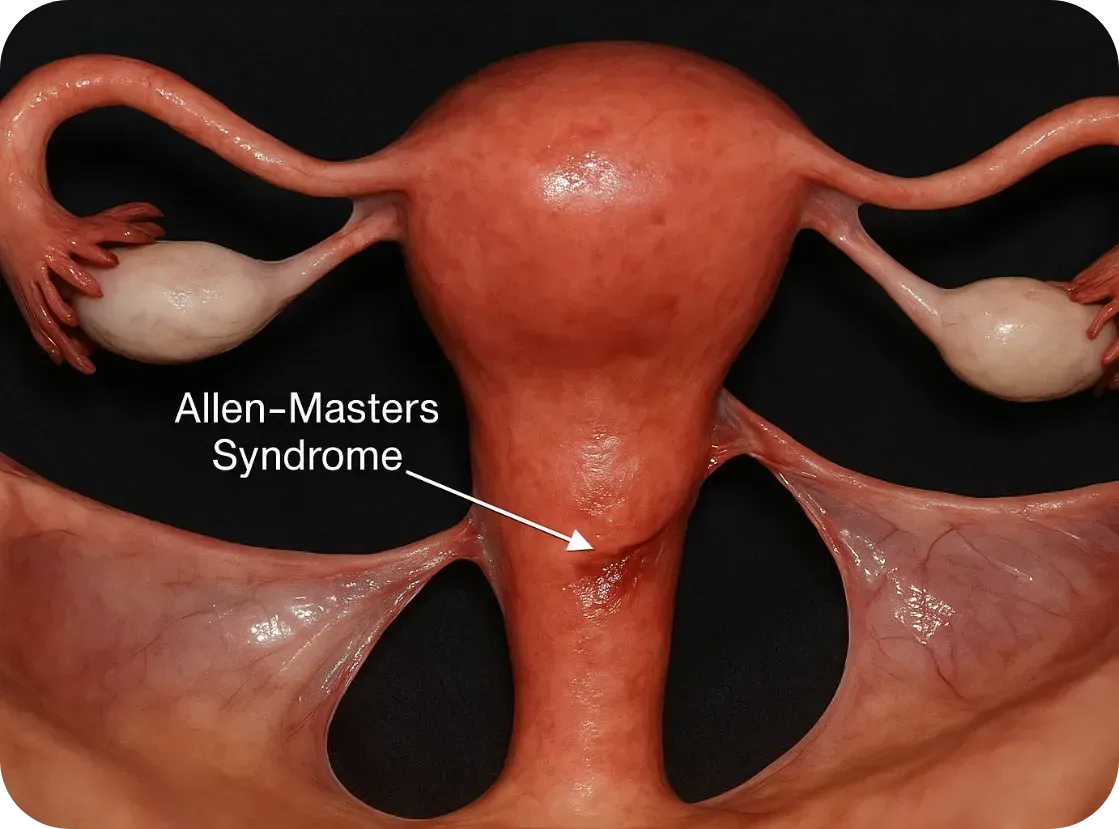
Allen-Masters Syndrome (AMS) refers to a condition where the ligaments that support the uterus become torn or stretched, often due to trauma or childbirth. The damage causes the uterus to become hypermobile, or “floppy,” which can lead to chronic pelvic pain, abnormal uterine positioning, and a range of gynecological symptoms.
First described in the 1950s by gynecologists Allen and Masters, the syndrome was initially observed in women who experienced difficult or forceful deliveries. However, it's now known that other pelvic trauma—such as surgeries, repeated inflammation, or even invasive endometriosis—can also play a role.
How It Feels: The Symptoms
The symptoms of AMS often overlap with other pelvic disorders, including endometriosis, which makes it incredibly hard to diagnose:
• Chronic pelvic pain, especially on one side
• Pain during intercourse (dyspareunia)
• A feeling of “heaviness” or dragging in the pelvis
• Irregular bleeding or spotting
• Referred pain to the lower back or legs
• Pain made worse by certain movements or positions
These symptoms can persist even after surgery for endometriosis or fibroids, leaving women frustrated and wondering why their treatments didn’t work.
The Complication with Endometriosis
Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.

Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.
Here’s how:
1. Mimicking or Masking Each Other
AMS pain can feel nearly identical to endometriosis. In laparoscopic surgery, torn ligaments or peritoneal defects might be mistaken for endometriosis—or missed entirely.
2. Worsening Each Other
The uterine instability caused by AMS may increase friction and inflammation in the pelvis, potentially exacerbating endometriosis symptoms. Likewise, the invasive nature of endometriosis can weaken uterine ligaments, creating a cycle of worsening pain.
3. Delaying Diagnosis
Because AMS isn’t well known, many surgeons focus only on excising visible endometriosis lesions. If ligament tears or pelvic instability aren’t also addressed, pain may persist despite "successful" surgery.
4. Influencing Fertility
While endometriosis is a known contributor to infertility, AMS can add to the challenge by altering the position of the uterus, interfering with sperm transport, or making embryo implantation more difficult.
Diagnosis: Why It’s Often Missed
AMS is best diagnosed through clinical examination and often requires a high index of suspicion from an experienced gynecologic surgeon. Imaging like MRI or ultrasound may not show ligament damage clearly. In some cases, laparoscopic exploration is the only way to confirm it, by observing a hypermobile uterus or peritoneal defects (like dimples or windows in the pelvic lining).
Unfortunately, many OB/GYNs are not trained to look for Allen-Masters Syndrome, which means it’s often overlooked—especially in patients already diagnosed with endometriosis
What Can Be Done?
If AMS is suspected, the treatment may include:
• Pelvic physical therapy to support surrounding muscles and reduce pain
• Surgical repair or suspension of the damaged ligaments, often during laparoscopy
• Pain management strategies including nerve blocks or hormonal regulation if endometriosis is also present
• Lifestyle modifications to reduce strain on the pelvis (avoiding certain exercises, managing constipation, etc.)

The Takeaway
Allen-Masters Syndrome may not be as well-known as endometriosis, but its impact is very real—especially for women who feel like they've tried everything and still have no answers.
If you’ve had surgery for endometriosis and your pain persists, or if your symptoms don’t quite fit the typical endo profile, it might be worth asking your doctor about Allen-Masters Syndrome.
Women deserve full answers—not partial relief.
Sources & Further Reading
• Howard FM. (2003). Chronic Pelvic Pain. Obstetrics and Gynecology
• Vercellini P et al. (2006). Chronic pelvic pain: pathogenesis and therapy. Best Practice & Research Clinical Obstetrics and Gynaecology
• Tu FF et al. (2017). Beyond Endometriosis: Recognizing and Treating Comorbid Pelvic Pain Disorders. Clinical Obstetrics and Gynecology
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Neuroangiogenesis: Nerves & Blood Vessels Fueling Endo
How Nerves and Blood Vessels Fuel Endometriosis: Understanding Neuroangiogenesis

When we think of endometriosis, we often imagine painful periods, reproductive complications, or fatigue. But beneath these symptoms lies a deeper, more complex process—one that helps explain why this condition is so painful, why it often gets worse over time, and why standard treatments don’t always work.
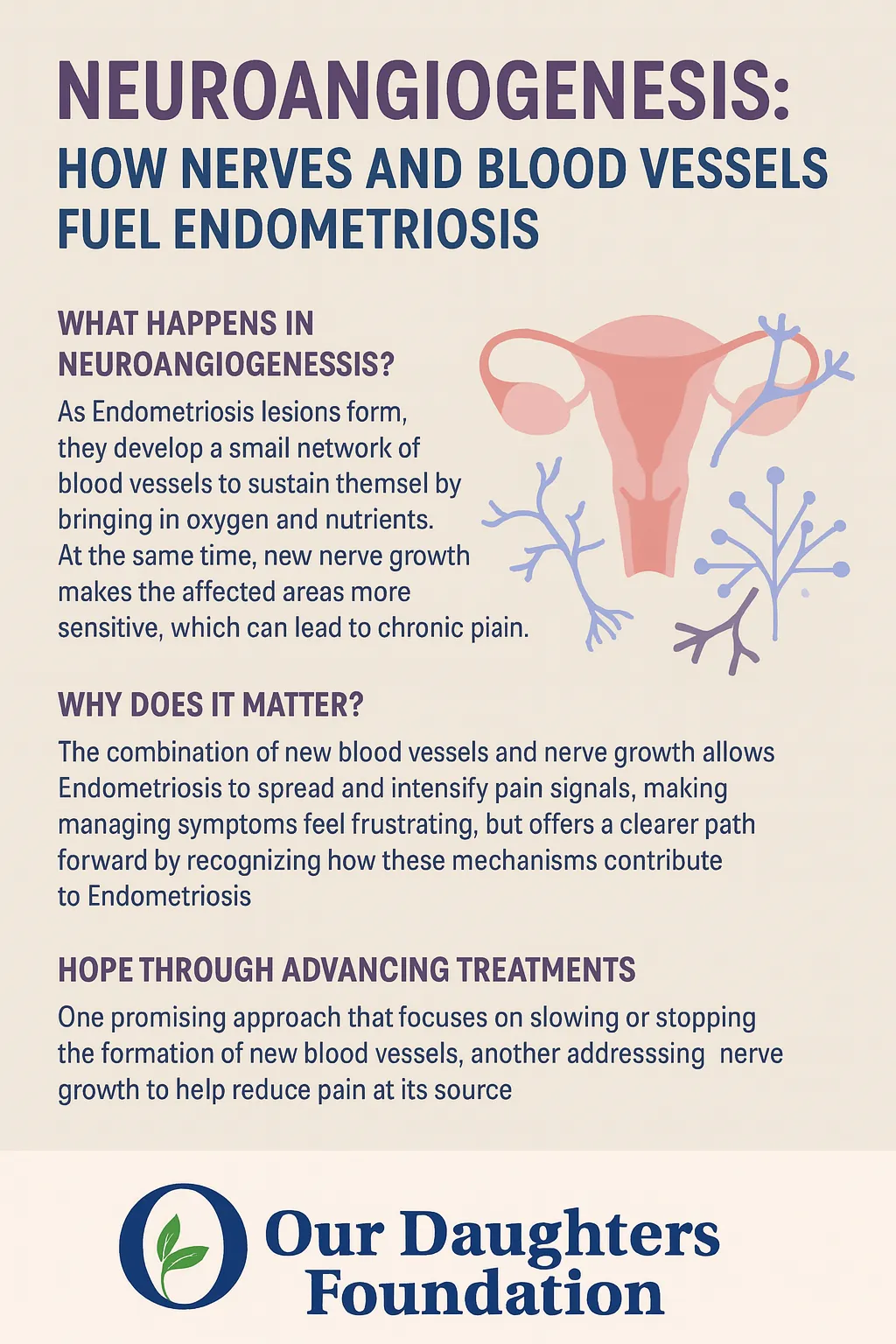
That process is called neuroangiogenesis—a mouthful of a word that simply means the simultaneous growth of new nerves (neuro-) and blood vessels (-angiogenesis). And it’s changing the way experts understand and treat endometriosis.
What Is Neuroangiogenesis?
Dr. Vimee Bindra, a leading gynecologist and endometriosis specialist, puts it plainly:
“Neuroangiogenesis fuels the pain of endometriosis.”
In her article, she explains that endometriotic lesions aren’t passive—they actively create their own support systems. These lesions grow tiny blood vessels that bring in oxygen and nutrients, helping them survive even in hostile environments like the pelvis, bowel, bladder, or abdominal wall. But even more troubling, they also stimulate nerve growth—making the affected areas more sensitive and painful.
This explains why pain in endometriosis isn’t limited to menstruation. For many women, it’s constant. It flares during ovulation. It radiates into the legs or back. It worsens with movement, digestion, or intimacy.
Why? Because it’s not just inflammation—it’s nerve-driven pain. The same biological mechanisms that help our body heal after injury are being hijacked by endometriosis lesions to sustain and spread the disease.
The Science Behind It
Research supports this dual growth model:
Studies have found that vascular endothelial growth factor (VEGF), which encourages new blood vessel formation, is overproduced in endometriotic tissue.
At the same time, nerve growth factor (NGF) is elevated, helping lesions become densely innervated and hypersensitive.
In fact, some studies report that lesions have 10 to 50 times more nerve fibers than similar tissue in people without endometriosis.
This combination of angiogenesis and neurogenesis makes endometriosis uniquely painful—and uniquely difficult to treat with one-size-fits-all approaches.
Why It Matters
Pain is not just a symptom of endometriosis—it’s a sign of progression.
Neuroangiogenesis helps explain why:
Endometriosis pain doesn’t always correlate with the size of lesions.
Pain can continue even after menopause or a hysterectomy.
Hormonal treatments alone often fail to fully relieve symptoms.
Dr. Bindra emphasizes that neuroangiogenesis helps us reframe endometriosis not just as a hormonal or reproductive issue, but as a neurovascular condition—one that affects the immune system, the nervous system, and the vascular system all at once.
Understanding this has the potential to unlock better, longer-lasting solutions.
A New Direction for Treatment
This evolving science is already inspiring a shift in how endometriosis is treated:
1. Anti-Angiogenic Therapies
By targeting VEGF and other blood vessel growth signals, researchers hope to “starve” lesions and stop them from spreading. Some cancer drugs are being investigated for this purpose, including bevacizumab, which blocks VEGF.
2. Nerve-Targeted Treatments
Medications that calm overactive nerves—such as gabapentin, pregabalin, or even newer biologics aimed at NGF—may help reduce pain at its neurological source.
3. Precision Surgery
Excision surgery done by skilled specialists—especially when guided by lesion-mapping tools like the ENZIAN classification—can remove deep, infiltrating lesions and decompress trapped nerves. This type of surgery is different from ablation and requires specialized expertise, but it can offer significant relief.
As Dr. Bindra notes in her clinical work, identifying the exact location and depth of lesions—especially those invading nerves—is critical for improving surgical outcomes.
Hope on the Horizon
At Our Daughters Foundation, we believe that informed care is empowered care. And understanding neuroangiogenesis gives us all a better framework for navigating endometriosis.
It helps patients explain their pain.
It helps doctors pursue more targeted treatments.
And it helps researchers continue moving toward real, long-term solutions.
You are not imagining your pain. You are not overreacting. You are not alone.
“The more we learn about how endometriosis builds its own nerve and blood supply, the closer we get to stopping it at the source.” – Dr. Vimee Bindra
References
Dr. Vimee Bindra
“Neuroangiogenesis: How Nerves and Blood Vessels Fuel Endometriosis”
https://www.drvimeebindra.com/neuroangiogenesis-how-nerves-and-blood-vessels-fuel-endometriosis/Dr. Vimee Bindra (LinkedIn)
Quote: “Neuroangiogenesis fuels the pain of endometriosis…”
https://www.linkedin.com/posts/dr-vimee-bindra-basu-7514765b_letstalkendo-endometriosisawarenessmonth-activity-7305270488694501381-KtCYTokushige N, Markham R, Russell P, Fraser IS
“Nerve fibers in peritoneal endometriosis”
Human Reproduction, 2006.
https://doi.org/10.1093/humrep/del009Taylor RN, Yu J, Torres PB, Schickedanz AC, Park JK, Mueller MD
“Mechanistic and therapeutic implications of angiogenesis in endometriosis”
Reproductive Sciences, 2020.
https://doi.org/10.1177/1933719119899937Arnold J, Barcena de Arellano ML, Rüster C, et al.
“Immunologic alterations in endometriosis: current understanding and future therapeutic implications”
Journal of Clinical Medicine, 2020.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7349441/Ferrero S, Gillott DJ, Remorgida V, et al.
“Use of antiangiogenic agents to treat endometriosis: a review”
Gynecological Endocrinology, 2010.
https://doi.org/10.3109/09513590903247814Bindra V, et al.
“Clinical Characteristics and Locations of Lesions in Patients with Endometriosis Using ENZIAN Classification”
Journal of Obstetrics and Gynaecology of India, 2025.
https://pubmed.ncbi.nlm.nih.gov/40390882/
