The Overlooked Link: Allen-Masters Syndrome and Endometriosis
How a Little-Known Condition Can Complicate Diagnosis and Treatment for Women in Pain
The Overlooked Link: Allen-Masters Syndrome and Endometriosis
How a Little-Known Condition Can Complicate Diagnosis and Treatment for Women in Pain
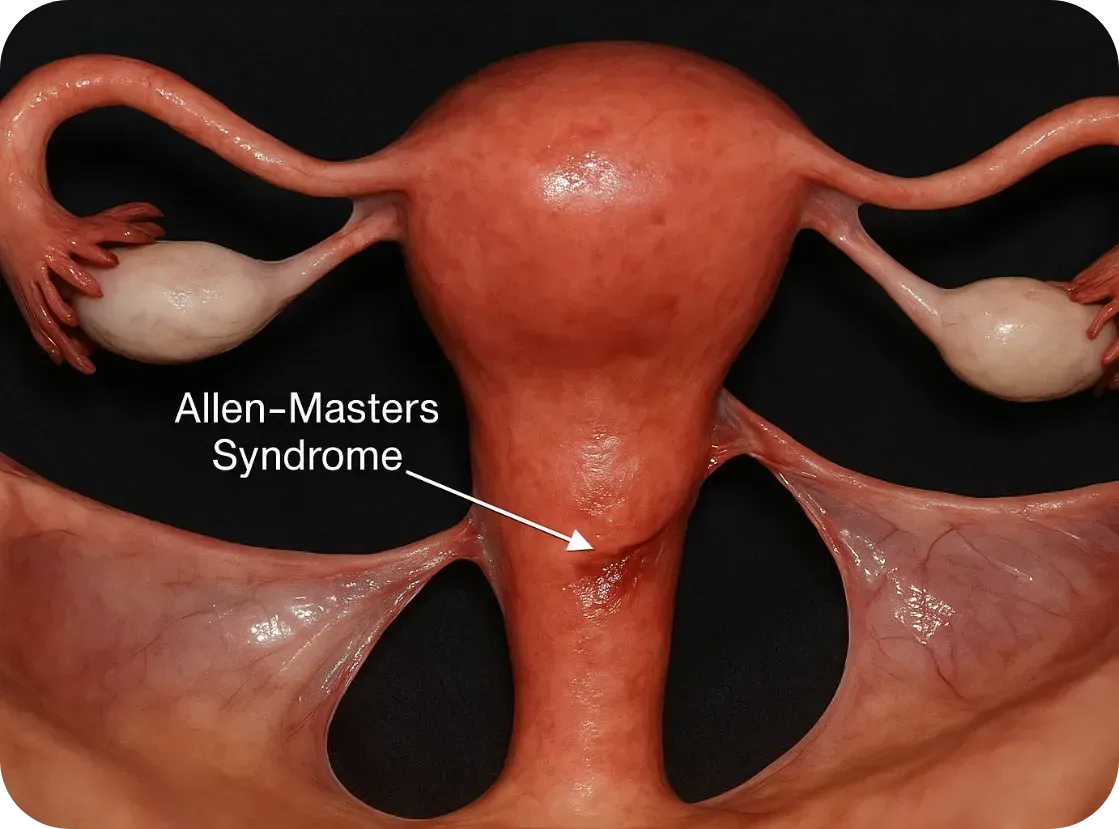
What Is Allen-Masters Syndrome?
Allen-Masters Syndrome (AMS) refers to a condition where the ligaments that support the uterus become torn or stretched, often due to trauma or childbirth. The damage causes the uterus to become hypermobile, or “floppy,” which can lead to chronic pelvic pain, abnormal uterine positioning, and a range of gynecological symptoms.
First described in the 1950s by gynecologists Allen and Masters, the syndrome was initially observed in women who experienced difficult or forceful deliveries. However, it's now known that other pelvic trauma—such as surgeries, repeated inflammation, or even invasive endometriosis—can also play a role.
How It Feels: The Symptoms
The symptoms of AMS often overlap with other pelvic disorders, including endometriosis, which makes it incredibly hard to diagnose:
• Chronic pelvic pain, especially on one side
• Pain during intercourse (dyspareunia)
• A feeling of “heaviness” or dragging in the pelvis
• Irregular bleeding or spotting
• Referred pain to the lower back or legs
• Pain made worse by certain movements or positions
These symptoms can persist even after surgery for endometriosis or fibroids, leaving women frustrated and wondering why their treatments didn’t work.
The Complication with Endometriosis
Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.

Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.
Here’s how:
1. Mimicking or Masking Each Other
AMS pain can feel nearly identical to endometriosis. In laparoscopic surgery, torn ligaments or peritoneal defects might be mistaken for endometriosis—or missed entirely.
2. Worsening Each Other
The uterine instability caused by AMS may increase friction and inflammation in the pelvis, potentially exacerbating endometriosis symptoms. Likewise, the invasive nature of endometriosis can weaken uterine ligaments, creating a cycle of worsening pain.
3. Delaying Diagnosis
Because AMS isn’t well known, many surgeons focus only on excising visible endometriosis lesions. If ligament tears or pelvic instability aren’t also addressed, pain may persist despite "successful" surgery.
4. Influencing Fertility
While endometriosis is a known contributor to infertility, AMS can add to the challenge by altering the position of the uterus, interfering with sperm transport, or making embryo implantation more difficult.
Diagnosis: Why It’s Often Missed
AMS is best diagnosed through clinical examination and often requires a high index of suspicion from an experienced gynecologic surgeon. Imaging like MRI or ultrasound may not show ligament damage clearly. In some cases, laparoscopic exploration is the only way to confirm it, by observing a hypermobile uterus or peritoneal defects (like dimples or windows in the pelvic lining).
Unfortunately, many OB/GYNs are not trained to look for Allen-Masters Syndrome, which means it’s often overlooked—especially in patients already diagnosed with endometriosis
What Can Be Done?
If AMS is suspected, the treatment may include:
• Pelvic physical therapy to support surrounding muscles and reduce pain
• Surgical repair or suspension of the damaged ligaments, often during laparoscopy
• Pain management strategies including nerve blocks or hormonal regulation if endometriosis is also present
• Lifestyle modifications to reduce strain on the pelvis (avoiding certain exercises, managing constipation, etc.)

The Takeaway
Allen-Masters Syndrome may not be as well-known as endometriosis, but its impact is very real—especially for women who feel like they've tried everything and still have no answers.
If you’ve had surgery for endometriosis and your pain persists, or if your symptoms don’t quite fit the typical endo profile, it might be worth asking your doctor about Allen-Masters Syndrome.
Women deserve full answers—not partial relief.
Sources & Further Reading
• Howard FM. (2003). Chronic Pelvic Pain. Obstetrics and Gynecology
• Vercellini P et al. (2006). Chronic pelvic pain: pathogenesis and therapy. Best Practice & Research Clinical Obstetrics and Gynaecology
• Tu FF et al. (2017). Beyond Endometriosis: Recognizing and Treating Comorbid Pelvic Pain Disorders. Clinical Obstetrics and Gynecology
What Is Allen-Masters Syndrome?
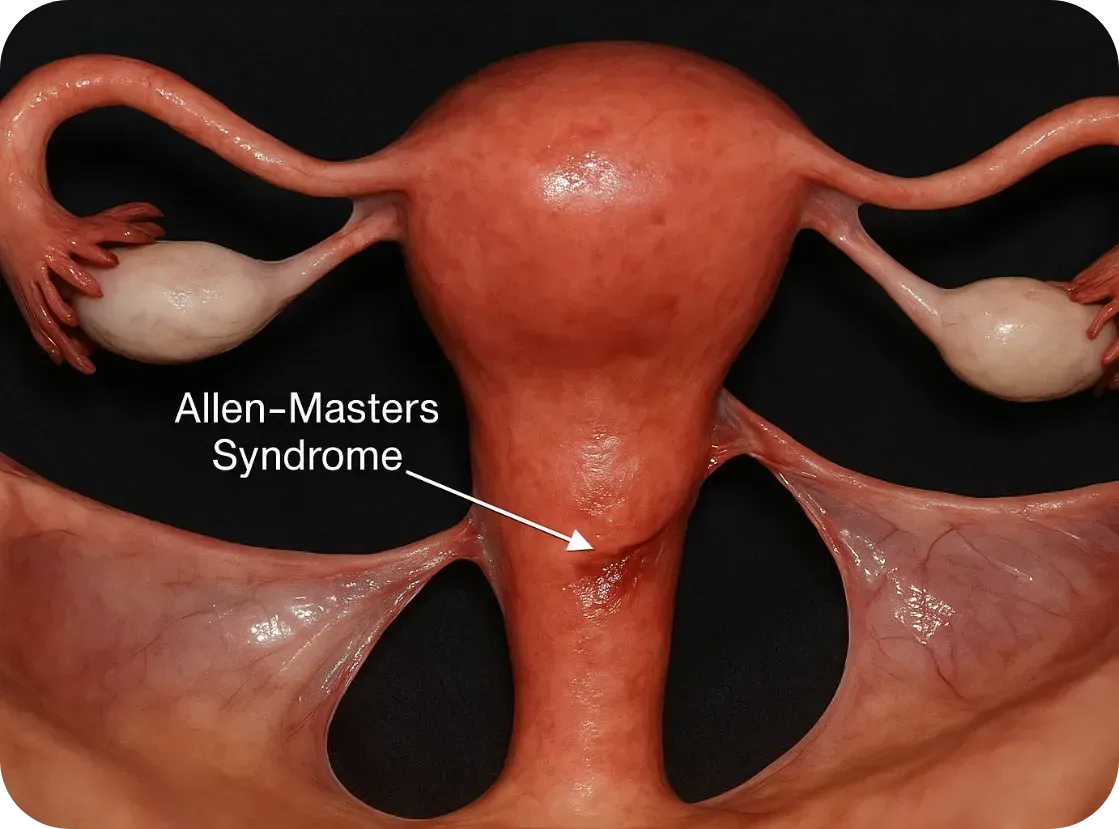
Allen-Masters Syndrome (AMS) refers to a condition where the ligaments that support the uterus become torn or stretched, often due to trauma or childbirth. The damage causes the uterus to become hypermobile, or “floppy,” which can lead to chronic pelvic pain, abnormal uterine positioning, and a range of gynecological symptoms.
First described in the 1950s by gynecologists Allen and Masters, the syndrome was initially observed in women who experienced difficult or forceful deliveries. However, it's now known that other pelvic trauma—such as surgeries, repeated inflammation, or even invasive endometriosis—can also play a role.
How It Feels: The Symptoms
The symptoms of AMS often overlap with other pelvic disorders, including endometriosis, which makes it incredibly hard to diagnose:
• Chronic pelvic pain, especially on one side
• Pain during intercourse (dyspareunia)
• A feeling of “heaviness” or dragging in the pelvis
• Irregular bleeding or spotting
• Referred pain to the lower back or legs
• Pain made worse by certain movements or positions
These symptoms can persist even after surgery for endometriosis or fibroids, leaving women frustrated and wondering why their treatments didn’t work.
The Complication with Endometriosis
Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.

Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.
Here’s how:
1. Mimicking or Masking Each Other
AMS pain can feel nearly identical to endometriosis. In laparoscopic surgery, torn ligaments or peritoneal defects might be mistaken for endometriosis—or missed entirely.
2. Worsening Each Other
The uterine instability caused by AMS may increase friction and inflammation in the pelvis, potentially exacerbating endometriosis symptoms. Likewise, the invasive nature of endometriosis can weaken uterine ligaments, creating a cycle of worsening pain.
3. Delaying Diagnosis
Because AMS isn’t well known, many surgeons focus only on excising visible endometriosis lesions. If ligament tears or pelvic instability aren’t also addressed, pain may persist despite "successful" surgery.
4. Influencing Fertility
While endometriosis is a known contributor to infertility, AMS can add to the challenge by altering the position of the uterus, interfering with sperm transport, or making embryo implantation more difficult.
Diagnosis: Why It’s Often Missed
AMS is best diagnosed through clinical examination and often requires a high index of suspicion from an experienced gynecologic surgeon. Imaging like MRI or ultrasound may not show ligament damage clearly. In some cases, laparoscopic exploration is the only way to confirm it, by observing a hypermobile uterus or peritoneal defects (like dimples or windows in the pelvic lining).
Unfortunately, many OB/GYNs are not trained to look for Allen-Masters Syndrome, which means it’s often overlooked—especially in patients already diagnosed with endometriosis
What Can Be Done?
If AMS is suspected, the treatment may include:
• Pelvic physical therapy to support surrounding muscles and reduce pain
• Surgical repair or suspension of the damaged ligaments, often during laparoscopy
• Pain management strategies including nerve blocks or hormonal regulation if endometriosis is also present
• Lifestyle modifications to reduce strain on the pelvis (avoiding certain exercises, managing constipation, etc.)

The Takeaway
Allen-Masters Syndrome may not be as well-known as endometriosis, but its impact is very real—especially for women who feel like they've tried everything and still have no answers.
If you’ve had surgery for endometriosis and your pain persists, or if your symptoms don’t quite fit the typical endo profile, it might be worth asking your doctor about Allen-Masters Syndrome.
Women deserve full answers—not partial relief.
Sources & Further Reading
• Howard FM. (2003). Chronic Pelvic Pain. Obstetrics and Gynecology
• Vercellini P et al. (2006). Chronic pelvic pain: pathogenesis and therapy. Best Practice & Research Clinical Obstetrics and Gynaecology
• Tu FF et al. (2017). Beyond Endometriosis: Recognizing and Treating Comorbid Pelvic Pain Disorders. Clinical Obstetrics and Gynecology
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
New Breakthroughs For Endometriosis

Hope on the Horizon: Breakthroughs in Endometriosis Research
Living with endometriosis or PCOS or fibroids (or any of the other hormone related, immune system diseases) can feel isolating, frustrating, and hopeless, especially for women who are actively fighting symptoms. We have previously highlighted the delay, dismissal and pain that is part of the experience for many of these women. BUT we also want to bring hope by saying that the landscape is starting to shift. Across the globe, researchers are unlocking new discoveries, philanthropists are investing boldly in women’s health, and for the first time in decades, there’s momentum toward real change. We hope this fills you with HOPE today and helps you to know that you are seen and cared for!
Here’s a look at some of the most hopeful developments reshaping the future of endometriosis care — and why we’re optimistic. (AND why we are doing our own research to know the best and most impactful places to invest our dollars!)
New Science Lighting the Way
Moving beyond hormones and surgery
Most current endometriosis treatments rely on hormonal suppression or invasive surgery — options that often come with serious side effects and don’t prevent recurrence or offer a cure.
But a new wave of research is aiming to change that.
Dichloroacetate (DCA), a metabolic drug once used for mitochondrial disorders, is showing surprising promise. In early clinical trials, it reduced lesion size and eased pain in many participants.
“This is the first time we’ve seen a drug target the energy metabolism of endometriosis cells. It’s a potential game-changer,”
— Professor Andrew Horne, University of Edinburgh
HMI-115, a monoclonal antibody targeting the prolactin receptor, is showing significant reductions in pain in Phase II trials.
“The fact that it’s non-hormonal and well tolerated could transform quality of life for millions,”
— Dr. Thomas D’Hooghe, Global Head of Reproductive Medicine R&D at Merck
More than 20 novel therapies are in development, many focused on immune and inflammatory pathways rather than hormones alone. This could lead to disease-modifying treatments, not just symptom control.
Faster, earlier diagnosis
Delays of 7–10 years from symptom onset to diagnosis are still common. That may soon change.
Big-data work at UCSF has identified patterns in millions of health records that could flag endometriosis earlier.
“We’re using artificial intelligence to see what no single doctor could spot in a lifetime,”
— Dr. Marina Sirota, UCSF Institute for Computational Health Sciences
In Australia, researchers are testing a blood-based biomarker panel that could detect endometriosis non-invasively.
New AI-assisted MRI tools are learning to identify endometriosis lesions with accuracy that rivals expert radiologists.
Dedicated research hubs
In May 2025, the Seckin Endometriosis Research Center opened at Cold Spring Harbor Laboratory, powered by a $10 million gift from the Endometriosis Foundation of America (EndoFound) and matched with another $10 million in institutional funding.
“We are building the infrastructure that has been missing in this field for decades. This is how you accelerate cures,”
— Dr. Bruce Stillman, President, Cold Spring Harbor Laboratory
Philanthropy Is Fueling Breakthroughs
After decades of neglect, private donors are helping rewrite the story of women’s health.
The Bill & Melinda Gates Foundation has pledged $2.5 billion through 2030 toward R&D in women’s health, explicitly including gynecologic conditions like endometriosis.
WHAM (Women’s Health Access Matters) has launched its annual Edge Awards to fund early-career researchers focused on endometriosis, PCOS, and menopause.
The Ainsworth family in Australia donated $50 million to launch the Ainsworth Endometriosis Research Institute at the University of New South Wales — the largest known single gift for endometriosis research to date, with the goal of accelerating the understanding, diagnosis and treatment of endometriosis through “integrated research and global collaboration.”
Melinda Gates donated $100 Million to women’s health in order to accelerate research. She emphasized what so many of us have known and live with the consequences of: women’s diseases have been neglected.
This surge in philanthropy is helping fill the gap where public funding has long fallen short. And the list above is not complete, there are many smaller efforts (like Our Daughters Foundation) that seek to fund research, grants for care, and raise awareness.
“Private investment is finally catching up to the urgency patients have always felt. These dollars are helping researchers pursue the bold, risky ideas that government grants often overlook,”
— Dr. Stacey Missmer, Harvard T.H. Chan School of Public Health
Stories of Hope
Beyond the data and dollars, these breakthroughs are already changing lives.
Ella, diagnosed at 14, was one of the youngest participants in the EPiC DCA trial. After years of missing school and friends, she finally began to get her life back.
“It’s like someone turned the volume down on my pain. I can go to class, see friends, be me again.”
Marisol, who endured five surgeries before finding relief with a newer oral therapy, says:
“For the first time in years, I’m planning my future without fear that pain will ruin it.”
We have also featured stories of hope on our pages to show you that you are not alone in your suffering and we are getting closer to understanding this disease.
🌱 Why We’re Hopeful
Endometriosis research is moving from a trickle to a tide, it’s a slow tide and we have a ways to go, but we are moving in the right direction. More of us are making noise, advocating and giving so that we can make a difference now and for our daughters in the future.
New, non-hormonal therapies are emerging.
Faster, less invasive diagnostics are within reach.
Philanthropy and private investment are pouring unprecedented resources into this space.
And most importantly, patients’ voices are finally driving the agenda.
At Our Daughters Foundation, we believe this momentum is just the beginning. The more we invest in understanding this disease — from immune pathways to diagnostic tools — the faster we can build a future where girls and women no longer lose years to pain. It’s a great time to get involved and actually see positive outcomes!
Join the Momentum
Every gift matters. Every conversation matters.
Together, we can help ensure this moment becomes a movement — and that every daughter has a future free from these often debilitating conditions and diseases.
