The Overlooked Link: Allen-Masters Syndrome and Endometriosis
How a Little-Known Condition Can Complicate Diagnosis and Treatment for Women in Pain
The Overlooked Link: Allen-Masters Syndrome and Endometriosis
How a Little-Known Condition Can Complicate Diagnosis and Treatment for Women in Pain
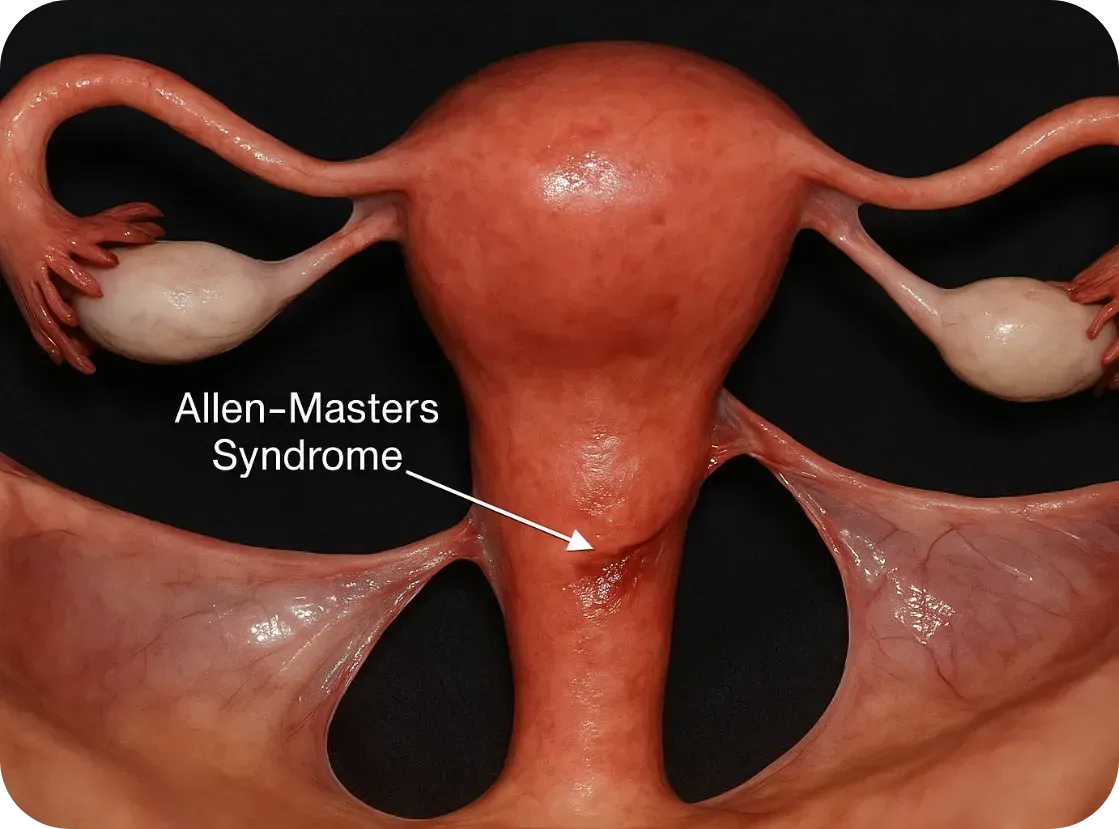
What Is Allen-Masters Syndrome?
Allen-Masters Syndrome (AMS) refers to a condition where the ligaments that support the uterus become torn or stretched, often due to trauma or childbirth. The damage causes the uterus to become hypermobile, or “floppy,” which can lead to chronic pelvic pain, abnormal uterine positioning, and a range of gynecological symptoms.
First described in the 1950s by gynecologists Allen and Masters, the syndrome was initially observed in women who experienced difficult or forceful deliveries. However, it's now known that other pelvic trauma—such as surgeries, repeated inflammation, or even invasive endometriosis—can also play a role.
How It Feels: The Symptoms
The symptoms of AMS often overlap with other pelvic disorders, including endometriosis, which makes it incredibly hard to diagnose:
• Chronic pelvic pain, especially on one side
• Pain during intercourse (dyspareunia)
• A feeling of “heaviness” or dragging in the pelvis
• Irregular bleeding or spotting
• Referred pain to the lower back or legs
• Pain made worse by certain movements or positions
These symptoms can persist even after surgery for endometriosis or fibroids, leaving women frustrated and wondering why their treatments didn’t work.
The Complication with Endometriosis
Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.

Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.
Here’s how:
1. Mimicking or Masking Each Other
AMS pain can feel nearly identical to endometriosis. In laparoscopic surgery, torn ligaments or peritoneal defects might be mistaken for endometriosis—or missed entirely.
2. Worsening Each Other
The uterine instability caused by AMS may increase friction and inflammation in the pelvis, potentially exacerbating endometriosis symptoms. Likewise, the invasive nature of endometriosis can weaken uterine ligaments, creating a cycle of worsening pain.
3. Delaying Diagnosis
Because AMS isn’t well known, many surgeons focus only on excising visible endometriosis lesions. If ligament tears or pelvic instability aren’t also addressed, pain may persist despite "successful" surgery.
4. Influencing Fertility
While endometriosis is a known contributor to infertility, AMS can add to the challenge by altering the position of the uterus, interfering with sperm transport, or making embryo implantation more difficult.
Diagnosis: Why It’s Often Missed
AMS is best diagnosed through clinical examination and often requires a high index of suspicion from an experienced gynecologic surgeon. Imaging like MRI or ultrasound may not show ligament damage clearly. In some cases, laparoscopic exploration is the only way to confirm it, by observing a hypermobile uterus or peritoneal defects (like dimples or windows in the pelvic lining).
Unfortunately, many OB/GYNs are not trained to look for Allen-Masters Syndrome, which means it’s often overlooked—especially in patients already diagnosed with endometriosis
What Can Be Done?
If AMS is suspected, the treatment may include:
• Pelvic physical therapy to support surrounding muscles and reduce pain
• Surgical repair or suspension of the damaged ligaments, often during laparoscopy
• Pain management strategies including nerve blocks or hormonal regulation if endometriosis is also present
• Lifestyle modifications to reduce strain on the pelvis (avoiding certain exercises, managing constipation, etc.)

The Takeaway
Allen-Masters Syndrome may not be as well-known as endometriosis, but its impact is very real—especially for women who feel like they've tried everything and still have no answers.
If you’ve had surgery for endometriosis and your pain persists, or if your symptoms don’t quite fit the typical endo profile, it might be worth asking your doctor about Allen-Masters Syndrome.
Women deserve full answers—not partial relief.
Sources & Further Reading
• Howard FM. (2003). Chronic Pelvic Pain. Obstetrics and Gynecology
• Vercellini P et al. (2006). Chronic pelvic pain: pathogenesis and therapy. Best Practice & Research Clinical Obstetrics and Gynaecology
• Tu FF et al. (2017). Beyond Endometriosis: Recognizing and Treating Comorbid Pelvic Pain Disorders. Clinical Obstetrics and Gynecology
What Is Allen-Masters Syndrome?
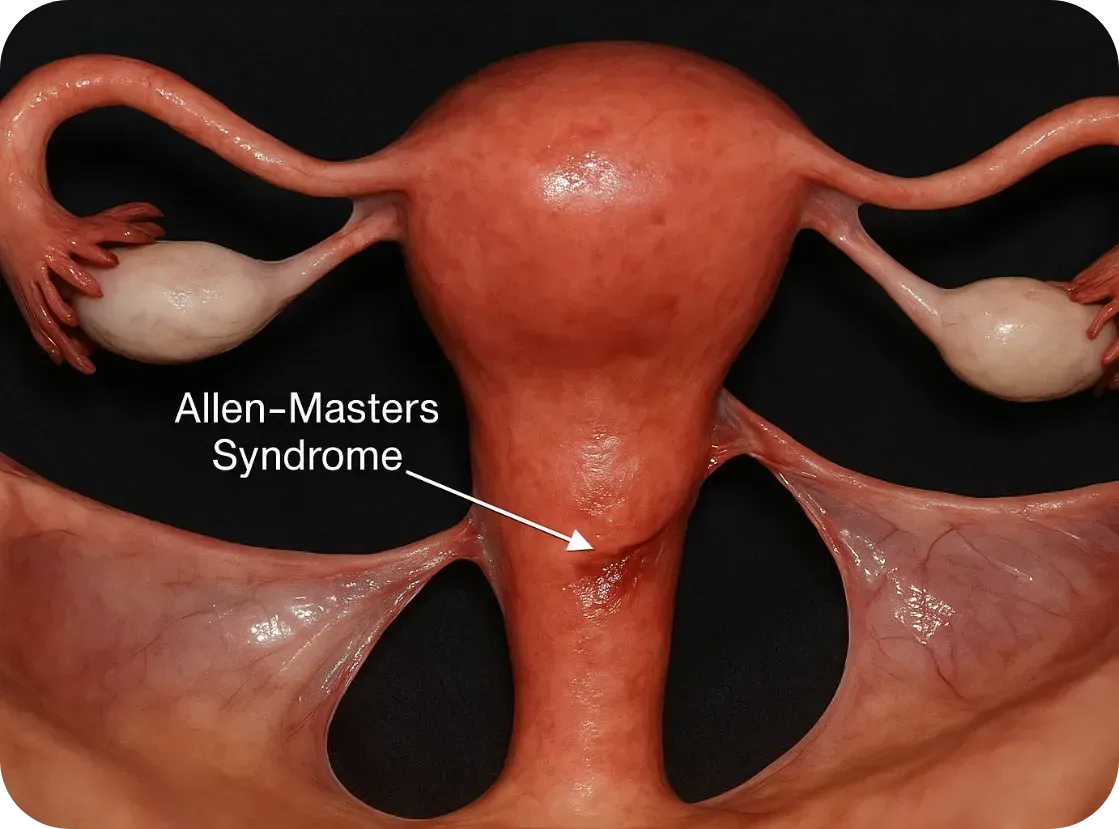
Allen-Masters Syndrome (AMS) refers to a condition where the ligaments that support the uterus become torn or stretched, often due to trauma or childbirth. The damage causes the uterus to become hypermobile, or “floppy,” which can lead to chronic pelvic pain, abnormal uterine positioning, and a range of gynecological symptoms.
First described in the 1950s by gynecologists Allen and Masters, the syndrome was initially observed in women who experienced difficult or forceful deliveries. However, it's now known that other pelvic trauma—such as surgeries, repeated inflammation, or even invasive endometriosis—can also play a role.
How It Feels: The Symptoms
The symptoms of AMS often overlap with other pelvic disorders, including endometriosis, which makes it incredibly hard to diagnose:
• Chronic pelvic pain, especially on one side
• Pain during intercourse (dyspareunia)
• A feeling of “heaviness” or dragging in the pelvis
• Irregular bleeding or spotting
• Referred pain to the lower back or legs
• Pain made worse by certain movements or positions
These symptoms can persist even after surgery for endometriosis or fibroids, leaving women frustrated and wondering why their treatments didn’t work.
The Complication with Endometriosis
Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.

Endometriosis and Allen-Masters Syndrome can coexist—and when they do, they complicate each other.
Here’s how:
1. Mimicking or Masking Each Other
AMS pain can feel nearly identical to endometriosis. In laparoscopic surgery, torn ligaments or peritoneal defects might be mistaken for endometriosis—or missed entirely.
2. Worsening Each Other
The uterine instability caused by AMS may increase friction and inflammation in the pelvis, potentially exacerbating endometriosis symptoms. Likewise, the invasive nature of endometriosis can weaken uterine ligaments, creating a cycle of worsening pain.
3. Delaying Diagnosis
Because AMS isn’t well known, many surgeons focus only on excising visible endometriosis lesions. If ligament tears or pelvic instability aren’t also addressed, pain may persist despite "successful" surgery.
4. Influencing Fertility
While endometriosis is a known contributor to infertility, AMS can add to the challenge by altering the position of the uterus, interfering with sperm transport, or making embryo implantation more difficult.
Diagnosis: Why It’s Often Missed
AMS is best diagnosed through clinical examination and often requires a high index of suspicion from an experienced gynecologic surgeon. Imaging like MRI or ultrasound may not show ligament damage clearly. In some cases, laparoscopic exploration is the only way to confirm it, by observing a hypermobile uterus or peritoneal defects (like dimples or windows in the pelvic lining).
Unfortunately, many OB/GYNs are not trained to look for Allen-Masters Syndrome, which means it’s often overlooked—especially in patients already diagnosed with endometriosis
What Can Be Done?
If AMS is suspected, the treatment may include:
• Pelvic physical therapy to support surrounding muscles and reduce pain
• Surgical repair or suspension of the damaged ligaments, often during laparoscopy
• Pain management strategies including nerve blocks or hormonal regulation if endometriosis is also present
• Lifestyle modifications to reduce strain on the pelvis (avoiding certain exercises, managing constipation, etc.)

The Takeaway
Allen-Masters Syndrome may not be as well-known as endometriosis, but its impact is very real—especially for women who feel like they've tried everything and still have no answers.
If you’ve had surgery for endometriosis and your pain persists, or if your symptoms don’t quite fit the typical endo profile, it might be worth asking your doctor about Allen-Masters Syndrome.
Women deserve full answers—not partial relief.
Sources & Further Reading
• Howard FM. (2003). Chronic Pelvic Pain. Obstetrics and Gynecology
• Vercellini P et al. (2006). Chronic pelvic pain: pathogenesis and therapy. Best Practice & Research Clinical Obstetrics and Gynaecology
• Tu FF et al. (2017). Beyond Endometriosis: Recognizing and Treating Comorbid Pelvic Pain Disorders. Clinical Obstetrics and Gynecology
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.
Join Us: Make a Difference Today
Your support can transform lives. Every donation helps us fund research, advocate for better care, and provide essential grants to women facing debilitating conditions.

My Story: Krissy Duenkel
Since I was around 12 years old, I’ve lived with excruciating periods. The kind of pain that made me miss days of school, doubled over in cramps, throwing up, and unable to function. I was told it was just “bad periods” and to tough it out — but what I was feeling was far from normal.
In college, things took a sharp turn for the worse. What used to be cyclical pain around my period became daily suffering. The cramps, back pain, leg pain — it never let up. I went from being a Division I athlete, pushing my body to its limits, to barely being able to get through a short walk. Eventually, I had to give up the sport I loved. I was trying to stay positive, trying to find answers. But every doctor’s visit felt like hitting a wall. I was dismissed, doubted, and gaslit time and time again.
After years of searching, an ER doctor finally said the word: endometriosis. I learned that the only way to confirm it was through exploratory surgery. I wasn’t ready yet — I tried everything else first: diets, medications, lifestyle changes. Nothing worked. The pain only got worse. I didn’t recognize myself anymore — I was just surviving.
Eventually, I couldn’t wait any longer. I had the surgery. They found endometriosis on multiple organs, along with adhesions that had fused parts of my organs to my pelvic wall. The relief after surgery was surreal. I experienced pain-free days for the first time in years — but only for about nine months.
Then it came back.
I tried another surgery a year later. And again, the cycle repeated. Short-lived relief, followed by a painful return. That brings me to today. I live with chronic pain — every day — without knowing when or if it will end.
But I’ve found a new purpose. Out of this suffering came something beautiful: Our Daughter’s Foundation, a mission born from pain but fueled by hope. I want a better future for others with this disease — one where they’re believed, diagnosed earlier, and given better options.
Today, my symptoms are complex and relentless. I experience pelvic congestion which results in extreme swelling in my lower abdomen, hips, back, and legs. It’s not just painful — it affects how I see myself. I struggle with body image, fatigue, nerve pain that radiates from my back down my legs, and daily flares triggered by even the smallest disruptions to my routine. I can’t exercise like I want to. I can’t live the way I used to. Intimacy is painful. Mornings are brutal. Nights are unpredictable.
This disease has taken a lot from me — but it hasn’t taken my voice. If you’re reading this and struggling, you’re not alone. I see you. And I’m fighting for a world where you don’t have to suffer in silence. -Krissy Duenkel
